ISSN: 0973-7510
E-ISSN: 2581-690X
Sexually transmitted disease (STD) consist of Neisseria gonoroheae, Chlamydia trachomatis, Syphilis and Trichomonyasis are a major public health concern. The prevalence of these organisms are increasing level because of homosexuality, migration and resistance to antibacterial agents and also usage of high technique for diagnosis of infection, according to WHO information 88 million people from 448 million which infected with STD, is Neisseria gonoroheae, whereas, Iran as a developing country have not complete prevalence information about Neisseria gonoroheae. In this study it has been tried to estimate the prevalence of Neisseria among Iranian women with phenotypin and genotyping methods. 300 specimens were enrolled in the present investigation which collected from women with genital problems. Dacron swab samples were cultured in chocolate agar in 37°C with 5-10% CO2 for 24-48 hours. Gram staining, oxidase and carbohydrate utilization tests were used to identify the isolated species. Extraction of DNA of all isolates recognize as Neisseria gonoroheae. PCR for amplification of 390 bp fragment of CPPB plasmid for confirmation of isolates were performed. From 300 specimens, 7 isolates recognize as Neisseria gonoroheae with culture and PCR methods. It means N. gonorrhoeae was detected in 2.6% cases which enrolled in this study. The study revealed that although primary report found no prevalence of gonorrohea in Iran but other study revealed different prevalence of bacteria in Iran, even in the recent studies, the results are very near to this result with consideration that gonoccocal infection have different sequelle in young age or pregnant women so it is very important that with culture or PCR methods, screening of bacteria should be done.
Phenotyping and Genotyping methods, STD, Neisseria gonoroheae.
The Neisseriae are gram-negative cocci that usually occur in pairs (diplococci). Neisseria gonorrhoeae (gonococci) is pathogenic for humans and typically are found associated with or inside polymorphonuclear cells. Gonococci attack mucous membranes of the genitourinary tract, eye, rectum, and throat, producing acute suppuration that may lead to tissue invasion, this is followed by chronic inflammation and fibrosis.in women cuses genitourinary tract infection with sequel of pelvic inflamatory disease, ectopic pregnancy.1,2
The prevalence of organism has increasing level because of homosexuality, migration and resistance to antibacterial agents, according to WHO information, 88 million people from 448 million which infected with STD is Neisseria gonoroheae, from 1990s th prevalence grow up in most countries of the world, but differs from one country to another (3,4), information of iran is spars and spread, so in this study it has beeb tried to investigate the perevalenc of gonoroheae in 3 groups of women, group 1 with cervicitis, group 2 reffer for (D&C) and group 3 women with spontaneous abortion. in order to have more and correct information about the prevalence of Neisseria gonorrhoeae with using of phenotyping (culture) and genotyping (PCR) methods.
During a 20 months study from September 2013 to March 2014, specimens were collected from 300 patients with genital problems who reffered to university of shahid beheshtie, Hospitals, Tehran, Iran. the specimens consist of 3 groups of women
Group 1: women with vaginal discharge ,abdominal pain ,bleeding (Cervicitis).
Group 2: women who reffered to hospital for (D&C).
Group 3: pregnant women who reffered for spontaneous abortion.
The mean age of group 1: was 36 year, group 2: 39 year, group 3: 27 year.
Specimens were collected with 2 Dacron swab for each patients, one for stuart medium , the other for gram staining. All smear of gram stain were seen for extracellular or intracellular G- diplococcic. Specimens in stwart medium were transport to chocolate agar and were placed in 37°C incubator, CO2 5% for 24-48 hours. Then oxidase test were done, for suspicious colonies utilaztion of sugars(glucose, lactose, maltose and sucrose) were used. (Table 1,2).
Table (1):
Result of Oxidaze test in3 groups.
Oxidaze pos |
Oxidaze Neg |
G – diplococci |
Number |
Specimen |
|---|---|---|---|---|
23 |
29 |
52 |
150 |
Vaginal discharge |
14 |
8 |
22 |
100 |
D&C |
16 |
3 |
19 |
50 |
Spontaneous abortion |
Table (2):
Result of utilization of sugars in Neisseria gonoroheae.
| Sucrose | Maltose | Lactose | Glucose | Oxidase pos specimen | ||||
|---|---|---|---|---|---|---|---|---|
| 20+ | 2- | 8- | 16+ | 2 – | 20+ | 23+ | Group 1=22 | |
| 12+ | 2- | 4- | 10+ | 2 – | 12+ | 14+ | Group 2=14 | |
| 14+ | 2- | 2- | 14+ | 2 – | 14+ | 16+ | Group 3=16 | |
group 1=vaginal discharge
group 2=D&C
group3=spontaneous abortion
For confirmation of isolates which recognize as Neisseria gonoroheae, extraction of 4.2 kb CPPB plasmid (5,6) by Nano plus plasmid Extraction kit BioNEER were done, PCR were performed with following format:
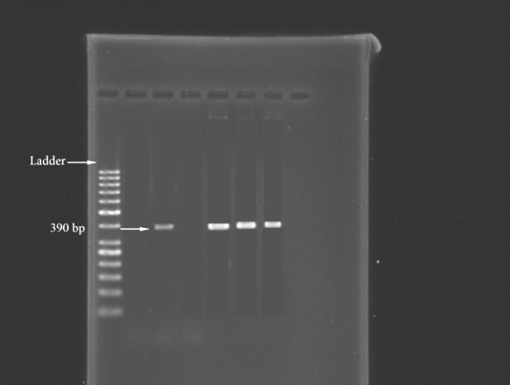 Figure: 390bp band of Neisseria gonoroheae
Figure: 390bp band of Neisseria gonoroheaePrimer Forward:5′ GCT ACG CAT ACCCGC GTT GC3′
Primer Reverse:5′ CGA AGA CCT TCG AGC AGA CA3′
PCR protocol: Primer forward=1µl, primer revers 1µl, DNA template 3
µl, Mastermix12 µl, ,8µl H20 ® Totalvolume =25µl
(94°C 30sec, 55°C 1min, 74°C 30sec) 94°C 5min
Lenght of product was 390bp by using 2% agaroze gel.
So the isolates which, with culture methods were Neisseria gonoroheae, with molecular method were confirmed as Neisseria gonoroheae too.
300 specimens were enrolled in this study consist of 150 cervicitis, 100 D&C, 50 spontanous abortion, 53 specimens were Oxidase and Catalase positive. The result of utilization of sugares according to table 2 revealed that 7 isolates were Glucose positive, Lactose, Maltose and Sucrose negative. which confirm that there were 7 isolates of Neisseria gonoroheae with phenotyping methods. Also with genotyping and molecular method and amplification of CPPB plasmid there were 7 isolates with 390bp band in PCR, which confirm of 7 isolates as Neisseria gonoroheae. So in our study with phenotyping and genotyping methos there were 7 isolates of Neisseria gonoroheae.
Table (3):
Frequency of Neisseria gonoroheae among 3 groups.
Frequency=% |
Positive for Neisseria gonoroheae |
Total number |
specimen |
|---|---|---|---|
2% |
N=3 |
150 |
group1= vaginal discharge |
2% |
N=2 |
100 |
group 2= D&C |
4% |
N=2 |
50 |
group3= spontaneous abortion |
This study sought to understand the prevalence of Neisseria gonoroheae among Iranian women who have genital problems by using of phenotyping (culture) and genotyping (PCR) methods. The result revealed that in 3 groups of women the prevalence of Neisseria gonoroheae was: group 1: 2%, group 2 :2%, and group 3:4%.The mean of 3 groups was 2.6%. according to WHO information. The prevalence of Neisseria gonorroheae has an increasing level from 1990s and differs from one country to another, also these informations indicate that the prevalence of gonoroheae between 2005 to 2008 grow up to 21% (4). In USA, overall rate of gonoroheae was 111.6 per 100000 population between 1989-2008.(5,7). In Africa there are a review article which consist of studies about prevalence of STD infection among African men and women, they reports the prevalence of Neisseria gonoroheae in women 5%, and in high risk groups like sex workers and women attending STIs clinics was between (10-31%).(6,8).
In Europe, a study has done with contribution of 12 European countries, an increasing rate in prevalence of N. gonorroheae observed from 1995 to 2002. In London ,wales and Northern Ireland gonorroheae diagnosed more than doubled between 1996 and 2001, in a study in Austria there was 414 cases of N. gonorroheae increase to 995 cases in 2002. with increasing rate both in men and women (7,9).
In neighborhood countries, like Turkey the Fahriye et al by using PCR found that the prevalence of gonorohae was3.7% among 370 endocervical samples (7,10), other study which has done in Palestine by using PCR and 213 endocervical specimens, revealed that the prevalence of gonoroheae was 1.4% (8,12), the other study in Bangladesh done by rahman et al, found that prevalence of gonorroheae in women with vaginal discharge was 3.8%, (9,13).
Studies which have done in recent years In Iran, cleared that in north west of Iran Zanjanprovince the prevalence of gonoroheae was 0.9% by using culture methods among pregnant and impregnant women.(10,14), in Babol north of Iran the prevalence was 0.2% by culture method (11,15), in Sabzevar the prevalence was o.9% by using triplex PCR (12,16), in Kermanshah west of Iran, the overall incidence of gonoroheae was 2.4% among 255 married women by doing PCR. ( 13,17), the other study which has done in Kashan found the prevalence of gonorrohae 2.38 % among 294 married women and using culture method (14,18) these studies which has done in recent years have similar and near result, specially the result of afrasiabi, (kashan) and akya (Kermanshah ) confirm our study, but in a study which performed by Batool Hossein Rashid et al, in Tehran, they examined 209 infertile women as cases and 170 pregnant women as controlle by using PCR for detection bacteria in urine ,they found no gonorroheae infection among the society which were selected (15,19), their result is oppose to other study which has done in iran, different result could because of the source of specimen which they selected, it is likely that vaginal and genital discharge are better source for searching bacteria in women than urine. with consideration that young women and female adolescents are more susceptible to STIs compared to the male due to their anatomy, so infection in women could have different sequle like ectopic pregnancy or pelvic inflammatory disease (PID), it is better to culture of vaginal discharge become a routin test for women especially in young age for diagnosis and treatment of gonococcal infection.
- Jawetz, Melnick, Adelberg’s .Medical Microbiology. Twenty-Sixth Edition. 2013,285-295,359-370.
- Mandell Douglas,Benneth, S.principles and practice of infectious Diseases, 2;seventh edition.2010,2443-2457.
- World Health Organization. WHO Features No 152, WHOGeneva, 1990.
- WHO. Global prevalence and incidence of selected curablesexually transmitted diseases: overview and estimates. WorldHealth Organization, Geneva (1995).
- 5. M. Bruisten S. M.,Noordhoek G. T. ,van den Brule A. J. C. ,B. Duim B. ,Boel C. H. E., Multicenter Validation of the cppB Gene as a PCR Target forDetection of Neisseria gonorrhoeae. Journal of clinical microbiology, 2004, 42(9); p. 4332–4334.
- Ho B. S , Feng W. G, Wong B. K., and Egglestone S. I. Polymerase chain reaction for the detection of Neisseria gonorrhoeae in clinical samples. J Clin Pathol. 1992; 45(5): 439–442.
- www.advocatesforyouth.org.
- LF Johnson, DJ Coetzee, RE Dorrington.Sentinel surveillance of sexually transmitted infections in South Africa: a review Sex Transm Infect 2005; 81: 287-293.
- Eksi F, Dikensoy E, Gayyurhan ED, Balci I, Balat O,Karsligil O, et al. The prevalence of Chlamydia trachomatis and Neisseria gonorrhoeae in theendocervical swab specimens of symptomatic,asymptomatic and infertile women in Turkey. ArchGynecol Obstet. 2011; 283: 1349-55.
- Farraj MA, Abusada GM, Saleem AM, Joaidi AY,Radad RM, Atrash HN, et al. Detection of Neisseria gonorrhoeae in Palestinian women using polymerasechain reaction. Asian Biomed. 2010; 4: 637-40.
- Rahman S, Garland S, Currie M, Tabrizi SN, Rahman M, Nessa K. Prevalence of Mycoplasma genitalium in health clinic attendees complaining of vaginal discharge in Bangladesh. Int J STD AIDS. 2008; 19:772–774.
- Baghchesaraei H, Amini B, Hossaini M. Prevalence of infection with Nisseria gonorrhoeae and Chlamydia trachomatis in women visitors of gynecology and obstetrics clinics in Zanjan Province of Iran. African Journal of Microbiology. 2011; 5:2447–2450.
- Bakhtiari A, Firoozjahi A. Chlamydia trachomatis infection in women attending health centres in Babol: prevalence and risk factors. East Mediterr Health J. 2007; 13: 1124–1131.
- Haghighi Hasanabad M, Bahador A, Mohammadzadeh M, Haghighi F. Prevalence of Chlamydia Trachomatis, Neisseria Gonorrhoeae and Ureaplasma Urealyticum in Pregnant Women of Sabzevar – Iran. Sex Transm Infect. 2013; 89:233–234.
- Alisha Akyaa, Hossein M, Olfati M, Mirnejad R, Mansur Altaha S, Rezaee M. The frequency of Chlamydia trachomatis and Neisseria gonorrhoeae infections among women in Kermanshah, Iran. Asian Biomedicine. 2013; 7: 681–685.
- Afrasiabi S, Moniri R, Samimi M, Mousavi SG. The frequency of Neisseria gonorrhoeae endocervical infection among female carrier and changing trends of antimicrobial susceptibility patterns in Kashan, Iran. Iran J Microbiol. 2014; 6(3): 194–197.
- Rashidi B, Chamani Tabriz L, Haghollahi F, Jeddi Tehrani M, Ramezanzadeh F, Rahimi Forooshani A, et al. Prevalence of Neisseria gonorrhea in Fertile and Infertile Women in Tehran. Medical Journal of Reproduction & Infertility. 2009; 9: 379–383.
© The Author(s) 2016. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.