ISSN: 0973-7510
E-ISSN: 2581-690X
Human monkeypox (now termed as the “Mpox”) was considered a geographically isolated disease until recently, but the current spread of the disease over 110 locations around the world has created an environment of fear. This study was thus conducted to evaluate the knowledge and apprehensions about the ongoing outbreak of Monkeypox among the medical students and nursing staff who can be a vital source of dissemination of knowledge to the general population. A semi-structured, self-administered questionnaire, was used in this cross-sectional offline study. The study population comprised Medical undergraduate students and nursing staff of a medical college situated in northern India. A total of 340 participants took part in the study comprising 302(88.8%) medical undergraduates and 38(11.1%) nursing staff. Overall, the knowledge of medical students and nursing staff was unsatisfactory. When the questionnaire data were analyzed only 17.05% of the participants had good knowledge, 20.58% had moderate knowledge and 65.78% had poor knowledge. Overall knowledge about the human monkeypox virus and disease was underwhelming. Medical students and nursing staff can be a vital source of dissemination of knowledge to the general population. In this era of emerging threats; to fill the knowledge gaps of the health care professionals’ strategies like continuing medical education, webinars, seminars, and workshops primarily focussing on better clinical, prevention, and control practices should be conducted frequently.
Mpox, Monkeypox Virus, Smallpox, Knowledge, Outbreak, Apprehension
Poxviridae have always been significant in human history. One of the scariest of Pox viruses which affected humans was smallpox with a high fatality rate of 3 out of 10. Those who survived usually had scars, which were sometimes severe. Although there are other pox viruses which affect humans but they cause mild illnesses or are limited to hosts other than humans. Recently, Monkeypox (now termed as the “Mpox”), which is primarily a disease of monkeys and other small mammals (like rope and sun squirrels, giant-pouched rats, African dormice) emerged in regions where it was not known before. After recovering from the COVID-19 pandemic, the emergence of Monkeypox was considered a new threat. The swift spread of the disease has caused an alarming situation globally with no certain answers about the severity of illness it may be causing and for the extent of spread.1,2
The Monkeypox virus belongs to the family poxviridae, subfamily Chordopoxvirinae, genus Orthopoxvirus and is an enveloped double-stranded DNA virus3. Although it belongs to the same family as smallpox, the disease. Like other pox viruses, MPXV is brick-shaped, with approximately 200-250 nm size, and is surrounded by a lipoprotein envelope.3-6
The virus was identified in 1958, accidentally in monkeys from lesions of a pox-like disease, and the disease acquired the term monkeypox. In 1970, the first human case of monkeypox was reported from the Democratic Republic of the Congo.3 Human cases are common in Central and West Africa, with a fatality rate of 5-10%.3,4 First outbreak outside Africa was reported in 2003, in the United States, with no case of human-to-human transmission.7,8 In contrast, an outbreak during the same time in the Republic of Congo where human transmission was noted.9 Discrete reports of outbreaks with no significant mortality had been reported in African Countries since then.10 However, since May 2022, many non-endemic states in European countries, the United States, Australia, Asia, and the Middle East reported monkeypox cases which raised the alarm.11
In India, first confirmed case was reported on 14, July 2022 from Kerela. India was the tenth country to report a monkeypox case in Asia and the first in South Asia. India reported five cases form Kerala and six from Delhi making a total of eleven confirmed cases of monkeypox.
Recent experiences of the general population and of the healthcare workers during the COVID-19 pandemic and the lineage of monkeypox to smallpox raised many concerns and fear of a pandemic with severe mortality or morbidity. This study was thus conducted to evaluate the knowledge and apprehensions about the ongoing outbreak of Monkeypox among the medical students and nursing staff who can be a vital source of dissemination of knowledge to the general population.
Study design
This cross sectional offline study was done to evaluate the knowledge and assess the apprehension for monkeypox during an outgoing outbreak among the medical undergraduates and the nursing staff at a tertiary care and teaching institution of North India. A semi structured, self administered questionnaire, was used to access the knowledge and apprehension about the monkeypox disease. The questionnaire was validated by face validity and a pilot study on 10% of the sample size. Identity of the respondents was not revealed and confidentiality was maintained throughout the entire process. Ethical clearance was obtained from the Institutional Ethical Committee, JNMCH, AMU.
Participants
The study population comprised of Medical undergraduate students (MBBS students from different phase of their study) and nursing staff of a medical college situated in northern India. A total of 38 responses were recorded from nursing staff and the remaining 302 from MBBS students.
Questionnaire
The questionnaire consisted of 22 questions assessing the knowledge regarding epidemiology, clinical manifestations, management and prevention. These questions consisted of two types of questions i) single correct answer ii) multiple correct answer; for questions that had single correct answer, 1 point was given for a correct response and 0 was given for a wrong response. In multiple correct answer type questions, 2 points were given for all correct responses, 1 point for partially correct response and 0 points were given when all responses were wrong. Using the Bloom’s cut off point, a score between of 0 and 18 was given the category of Low knowledge, score between 19-24 was considered moderate knowledge and a score above 24 was considered high knowledge. Three questions included were for assessing the apprehension and attitude of the participants. Two of these questions were supposed to be rated on on a 5-point Likert scale. Questionnaire was given to the consenting participants in person and 25 minutes were provided to complete it. The mean time for completing the questionnaire was 14 minutes.
Statistical analysis
Data were analysed using MedCalc developed by MedCalc Software (acacialaan 22, 8400 ostend, Belgium). Data were presented as frequency (percentage). [https://www.medcalc.org/calc/diagnostic_test.php]
A total of 340 participants took part in the study comprising 302(88.8%) medical undergraduates and 38(11.1%) nursing staff. Overall, the knowledge of medical students and nursing staff was unsatisfactory; with MBBS students scoring slightly better than the nursing staff. Gross deficiencies in knowledge were seen in some areas like the majority of the participants missed respiratory droplets as a mode of transmission; 45% of the missed lymphadenopathy as the clinical feature of the disease; 40.08% mentioned one skin lesion and one serum sample as the recommended sample to collect in monkeypox; 80.5% considered quarantine of contacts as infection prevention and control measure; 73.2% answered shaking of linen well before washing to remove all viruses when handling used bed linen from monkeypox patient as correct option; 35.2% thought that monkeypox patient is infectious till it feels well. (Table 1)
Table (1):
Table 1. Questionnaire with responses and results.
| S. No. | Question | Options | Response | Percentage (%) |
Response | Percentage (%) |
MBBS | Percentage (%) |
Nursing | Percentage (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Monkeypox in humans is | an infection with a virus circulating in all wildlife around the world | 167 | 49.11 | 167 | 49.11 | 157 | 51.98 | 10 | 26.31 |
| an infection with a virus circulating in wildlife in Central and West Africa | 112 | 32.94 | 112 | 32.94 | 97 | 32.11 | 15 | 39.47 | ||
| an infection with bacteria circulating in wildlife in Central and West Africa | 23 | 6.76 | 23 | 6.76 | 10 | 3.31 | 13 | 34.21 | ||
| none of the above | 38 | 11.17 | 38 | 11.17 | ||||||
| 2 | Monkeypox is a zoonosis, which means a disease which can spread | |||||||||
| from humans to animals | 38 | 11.17 | 38 | 11.17 | 29 | 9.6 | 9 | 23.68 | ||
| among animals in zoos | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| from animals to humans | 302 | 88.82 | 302 | 88.82 | 273 | 90.39 | 29 | 76.31 | ||
| 3 | Monkeypox can be transmitted by: (select all that apply) | body fluids | 267 | 78.52 | ac237 | 69.7 | 231 | 76.49 | 6 | 15.78 |
| lesion material | 288 | 84.7 | pc 103 | 30.29 | 71 | 23.5 | 32 | 84.21 | ||
| respiratory droplets | 103 | 30.29 | ||||||||
| contaminated materials and surfaces | 298 | 87.64 | ||||||||
| 4 | What are the main environmental and social factors for monkeypox emergence: | |||||||||
| civil unrest and poverty; climate change; expanding mosquito populations; cessation of smallpox vaccination; | 14 | 4.11 | 14 | 4.11 | 5 | 1.65 | 9 | 23.68 | ||
| deforestation; climate change; civil unrest and poverty; cessation of smallpox vaccination; | 174 | 51.17 | 174 | 51.17 | 158 | 52.31 | 16 | 42.1 | ||
| cessation of smallpox vaccination; climate change; expanding mosquito populations; overcrowding. | 152 | 44.7 | 152 | 44.7 | 139 | 46.02 | 13 | 34.21 | ||
| 5 | Which animals were reported to transmit monkeypox to humans (select all that apply) | |||||||||
| Bats | 52 | 15.29 | ac 149 | 43.82 | 142 | 47.01 | 7 | 18.42 | ||
| Monkeys | 265 | 77.94 | pc 162 | 47.64 | 144 | 47.68 | 18 | 47.36 | ||
| Rodents | 212 | 62.35 | aw 29 | 8.52 | 16 | 5.29 | 13 | 34.21 | ||
| Poultry | 69 | 20.29 | ||||||||
| 6 | One Health is an approach to developing policies, programmes, legislation, and research for the human-animal-environment interface in which different sectors work together to achieve better public health outcomes | |||||||||
| TRUE | 289 | 85 | 289 | 85 | 268 | 88.74 | 21 | 55.26 | ||
| FALSE | 51 | 15 | 51 | 15 | 34 | 11.25 | 17 | 44.73 | ||
| 7 | Monkeypox is characterized by: (select all that apply) | |||||||||
| Fever | 247 | 72.64 | ac 148 | 43.52 | 134 | 44.37 | 14 | 36.84 | ||
| Cough | 148 | 43.52 | pc 192 | 56.47 | 168 | 55.62 | 24 | 63.15 | ||
| Rash | 192 | 56.47 | ||||||||
| Swollen lymph nodes | 187 | 55 | ||||||||
| 8 | How long is the incubation period for human monkeypox? | |||||||||
| 5 to 13 days | 84 | 24.7 | 84 | 24.7 | 72 | 12 | 31.57 | |||
| 3 to 7 days | 37 | 10.88 | 37 | 10.88 | 30 | pc 219(64.41) | 7 | 18.42 | ||
| 5 to 21 days | 158 | 46.47 | 158 | 46.47 | 148 | aw 121(35.58) | 10 | 26.31 | ||
| 6 to 13 days | 61 | 17.94 | 61 | 17.94 | 52 | 9 | 23.68 | |||
| 9 | The rash in monkeypox progresses as follows | |||||||||
| macule, vesicle, papule, pustule, crust | 33 | 9.7 | 33 | 9.7 | 20 | 6.62 | 13 | 34.21 | ||
| papule, macule, vesicle, pustule, crust | 20 | 5.88 | 20 | 5.88 | 6 | 1.98 | 14 | 36.84 | ||
| macule, papule, vesicle, pustule, crust | 287 | 84.41 | 287 | 84.41 | 276 | 91.39 | 11 | 28.94 | ||
| 10 | The known complications of monkeypox include? (select all that apply) | |||||||||
| secondary bacterial infection | 245 | 72 | ac 118 | 34.7 | 115 | 38.07 | 3 | 7.89 | ||
| bleeding | 202 | 59.41 | pc
222 |
65.25 | 187 | 61.92 | 35 | 92.11 | ||
| bronchopneumonia | 198 | 58.23 | ||||||||
| blindness | 178 | 52.35 | ||||||||
| 11 | . Among the following statements, tick those which are correct: | |||||||||
| monkeypox and chickenpox both present with a rash on palms and soles | 268 | 78.82 | ac 139 | 40.88 | 137 | 45.36 | 2 | 5.26 | ||
| lymphadenopathy is generally present in monkeypox | 199 | 58.52 | pc 187 | 55 | 164 | 54.3 | 23 | 60.52 | ||
| Monkeypox rash lesions evolve through the stages of development at the same time | 213 | 62.64 | aw 14 | 4.11 | 1 | 0.33 | 13 | 34.21 | ||
| monkeypox rash is usually denser on the extremities than on the trunk | 187 | 55 | ||||||||
| 12 | The best diagnostic specimen to collect for laboratory confirmation of monkeypox is: | |||||||||
| tonsillar or nasopharyngeal swabs | 33 | 9.7 | 33 | 9.7 | 7 | 2.31 | 5 | 13.15 | ||
| sputum | 20 | 5.88 | 20 | 5.88 | 4 | 1.32 | 2 | 5.26 | ||
| skin lesions | 287 | 84.41 | 287 | 84.41 | 285 | 94.37 | 24 | 63.15 | ||
| serum | 10 | 2.94 | 10 | 2.94 | 3 | 0.9 | 7 | 18.42 | ||
| 13 | For laboratory confirmation of monkeypox, it is recommended to collect | |||||||||
| a single nasopharyngeal swab | 79 | 23.23 | 79 | 23.23 | 61 | 20.19 | 18 | 47.36 | ||
| at least two skin lesion samples from different sites of the body | 114 | 33.52 | 114 | 33.52 | 110 | 36.42 | 4 | 10.52 | ||
| one skin lesion sample and one serum sample | 139 | 40.88 | 139 | 40.88 | 126 | 41.72 | 13 | 34.21 | ||
| there is no need to collect samples as the clinical picture is sufficient | 8 | 2.35 | 8 | 2.35 | 5 | 1.65 | 3 | 7.89 | ||
| 14 | Infection prevention and control precautions for monkeypox include (select all that apply) | |||||||||
| use of personal protective equipment (PPE) when caring for patients | 257 | 75.58 | ac 68 | 20 | 47 | 15.56 | 21 | 55.26 | ||
| isolation of patients | 269 | 79.11 | pc 235 | 69.11 | 222 | 73.5 | 13 | 34.21 | ||
| quarantine of contacts | 274 | 80.58 | aw 37 | 10.88 | 33 | 10.92 | 4 | 10.52 | ||
| hand hygiene practices | 215 | 63.23 | ||||||||
| keeping at least one metre distance | 206 | 60.58 | ||||||||
| 15 | What personal protective equipment must be worn when caring for a patient with suspected or confirmed monkeypox or collecting specimens? | |||||||||
| gown, gloves | 14 | 4.11 | 14 | 4.11 | 11 | 3.64 | 3 | 7.89 | ||
| gown, gloves, surgical mask | 47 | 13.82 | 47 | 13.82 | 31 | 10.26 | 16 | 42.1 | ||
| gown, gloves, surgical mask, goggles | 279 | 82.05 | 279 | 82.05 | 260 | 86.09 | 19 | 50 | ||
| none of the above | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 16 | The following are possible long-term sequelae of monkeypox (select all that apply | |||||||||
| blindness | 288 | 84.7 | ac 138 | 40.58 | 132 | 43.7 | 6 | 15.78 | ||
| paralysis | 231 | 67.94 | pc 117 | 34.41 | 102 | 33.77 | 15 | 39.47 | ||
| scarring | 309 | 90.88 | aw 85 | 25 | 68 | 22.51 | 17 | 44.73 | ||
| loss of skin pigmentation | 214 | 62.94 | ||||||||
| 17 | When handling used bed linen from monkeypox patients we should? (select all that apply) | |||||||||
| shake it well before washing to remove all virus particles | 249 | 73.23 | ac 118 | 34.7 | 98 | 32.45 | 20 | 52.63 | ||
| store in a leak proof bag | 304 | 89.41 | pc 219 | 64.41 | 202 | 66.88 | 17 | 44.73 | ||
| wash separately and at high temperature | 268 | 78.82 | aw 3 | 0.8 | 2 | 0.66 | 1 | 2.63 | ||
| wear a medical mask and gloves and a clean gown to protect yourself | 254 | 74.7 | ||||||||
| 18 | How should you care for an extensive monkeypox rash? | |||||||||
| cover it with a wet towel | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| use cloxacillin or amoxicillin | 45 | 13.23 | 45 | 13.23 | 29 | 9.6 | 16 | 42.1 | ||
| keep it dry and clean; use antibiotics if needed for secondary infection | 295 | 86.76 | 295 | 86.76 | 273 | 90.39 | 22 | 57.89 | ||
| 19 | How long is a monkeypox patient infectious? | |||||||||
| until antibodies in the blood can be detected | 48 | 14.11 | 48 | 14.11 | 40 | 13.24 | 8 | 21.05 | ||
| until the crusts fall off and new skin has formed | 172 | 50.58 | 172 | 50.58 | 152 | 50.33 | 20 | 52.63 | ||
| until the person feels well | 120 | 35.29 | 120 | 35.29 | 110 | 36.42 | 10 | 26.31 | ||
| 20 | First case of monkeypox was detected in India in which State? | |||||||||
| Kerala | 257 | 75.58 | 257 | 75.58 | 241 | 79.8 | 16 | 42.1 | ||
| Delhi | 35 | 10.29 | 35 | 10.29 | 32 | 10.59 | 3 | 7.89 | ||
| Uttar Pradesh | 18 | 5.29 | 18 | 5.29 | 16 | 5.29 | 2 | 5.26 | ||
| Maharashtra | 30 | 8.82 | 30 | 8.82 | 13 | 4.3 | 17 | 44.73 | ||
| 21 | How apprehensive are you of getting monkeypox? | 1 (very unconcerned) | 58 | 17.05 | 58 | 17.05 | 50 | 16.55 | 8 | 21.05 |
| 2 (unconcerned) | 216 | 63.52 | 216 | 63.52 | 212 | 70.19 | 4 | 10.52 | ||
| 3 (neutral) | 31 | 9.11 | 31 | 9.11 | 19 | 6.29 | 12 | 31.57 | ||
| 4 (concerned) | 9 | 2.64 | 9 | 2.64 | 4 | 1.32 | 5 | 13.15 | ||
| 5 (very concerned) | 26 | 7.64 | 26 | 7.64 | 17 | 5.62 | 9 | 23.68 | ||
| 22 | Do you feel we are prepared to tackle monkeypox virus outbreak? | Yes | 52 | 15.29 | 52 | 15.29 | 48 | 15.89 | 4 | 10.52 |
| No | 288 | 84.7 | 288 | 84.7 | 254 | 84.1 | 34 | 89.47 | ||
| 23 | Can monkeypox outbreak become as severe as Covid-19? | 1 (very unlikely) | 67 | 19.7 | 67 | 19.7 | 50 | 16.55 | 17 | 44.73 |
| 2 (unlikely) | 53 | 15.58 | 53 | 15.58 | 50 | 16.55 | 3 | 7.89 | ||
| 3 (Neutral) | 118 | 34.7 | 118 | 34.7 | 110 | 36.42 | 8 | 21.05 | ||
| 4 (likely) | 34 | 10 | 34 | 10 | 29 | 9.6 | 5 | 13.15 | ||
| 5 (very likely) | 68 | 20 | 68 | 20 | 63 | 20.86 | 5 | 13.15 | ||
| 24 | Antibiotics are required in the management of mild monkeypox infection? | |||||||||
| Yes | 141 | 41.47 | 141 | 41.47 | 120 | 39.73 | 21 | 55.26 | ||
| No | 199 | 58.52 | 199 | 58.52 | 182 | 60.26 | 17 | 44.73 | ||
| 25 | Antivirals are required in the management of mild monkeypox infection? | |||||||||
| Yes | 183 | 53.82 | 183 | 53.82 | 168 | 55.62 | 15 | 39.47 | ||
| No | 157 | 46.17 | 157 | 46.17 | 134 | 44.37 | 23 | 60.52 | ||
*ac= all correct, pc= partially correct, aw= all wrong
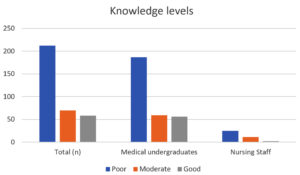
When the questionnaire data were analyzed only 17.05% of the participants had good knowledge, 20.58% had moderate knowledge and 65.78% had poor knowledge. (Table 2)(Figure 1)
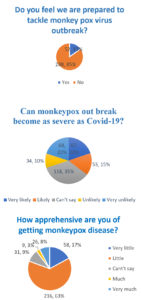
One of the factors which were assessed among the respondents was the apprehension and attitude towards monkeypox disease. 17.5% and 63.52% of respondents very unconcerned and unconcerned about getting monkeypox. Similarly, only 20% and 10% of them believed that its very likely and likely for monkeypox outbreak to become as severe as COVID-19 pandemic. However, majority (84.7%) felt that we are not prepared to tackle monkeypox outbreak (Figure 2).
Figure 2. Participants response to questions regarding the attitude and apprehension towards monkeypox disease
Table (2):
Knowledge levels of participants.
Level of Knowledge |
Score |
Total n (%age) |
Medical undergraduates n (%age) |
Nursing staff n (%age) |
|---|---|---|---|---|
Poor |
0-18 |
212(62.35) |
187(61.92) |
25(65.78) |
Moderate |
19-24 |
70(20.58) |
59(19.53) |
11(28.94) |
Good |
>24 |
58(17.05) |
56(18.54) |
2(5.26) |
n = total responses; %= percentage
Emerging and re-emerging pathogens have periodically caused epidemics and pandemics around the globe. The occurrence of these epidemics and pandemics has increased in frequency in recent times. Migrations of population, easy connectivity even to remote areas of the world, and frequent air travel may be responsible for such a phenomenon. As covid-19 pandemic has shown us, the general population, healthcare workers, and the administration all have to face several challenges during such periods. Each new outbreak, epidemic, or pandemic brings new fear and new anxiety. Lack of knowledge and awareness and an indifferent attitude can further worsen the problem. The monkeypox scare just as the covid-19 pandemic was diminishing in severity has questioned our preparedness for such occurrences. Healthcare workers are the best personnel to disseminate such knowledge about the disease in the community.
Assessment of the knowledge and apprehensions about the disease among the budding physicians and their supporting staff (nursing) will help us establish the basis of the measures to be taken to make aware the healthcare personnel and even the general population. In the present study medical undergraduates from different phases of their course and nursing staff answered a questionnaire regarding the monkeypox disease. It was seen that only 17.05% of the participants had good knowledge, whereas 20.58% and 62.35% we’re having moderate knowledge and poor knowledge. Medical undergraduates were slightly better than nursing staff. Similar studies conducted around the world also showed a gap in the knowledge of healthcare professionals and the general population. Harapan et al from Indonesia depicted that only 10.0% of general practitioners had good knowledge (80% Cut-off) which increased to 36.5% when the cut-off was lowered to 70%.12 Ricco et al noted a considerable knowledge gap among Italian physicians.13 Bates et al reported only 48.9% of clinicians from Ohio, USA answered the knowledge questions correctly.14 Studies conducted among the general population in Saudi Arabia 52%15 and university students of UAE 19.9%16 also had poor knowledge of the disease.
India is not endemic to Monkeypox or rather say there was no reported case of monkeypox before the recent outbreak. Therefore, for the healthcare professionals of India, this is a relatively new disease to encounter. Study and research of such uncommon diseases in the country may lack as compared to common/endemic diseases or diseases having global occurrence may be the reason for inadequate knowledge of the participants.
Zoonotic disease means it can spread from animals to humans; Monkeypox caused by Monkeypox virus, an Orthopoxvirus belongs to this category,17 and in the present study 88.8% of the respondents had good awareness of it being a zoonosis. However, only 33.94% of the participants could say that Monkeypox is an infection with virus circulating in the wildlife in Central and West Africa.18 Several factors have been speculated to be the underlying social and environmental factors for the increased frequency of monkeypox outbreaks namely increased susceptibility to monkeypox infection following the cessation of smallpox vaccination, poor countries affected by social unrest leading to dietary changes as consumption of animals as a protein source which are potential MPXV reservoirs, deforestation, easy air travel and increased population density.19 Expanding mosquito population does not affect monkeypox spread as it is not a vector borne disease, however 48.83% of the participants believed it to be as one of the factors facilitating the spread. According to CDC, although animal reservoir is unknown, small mammals (e.g. rope and sun squirrels, giant-pouched rats, African dormice) are thought to maintain the virus in the environments of West and Central Africa and despite its name Monkeys are not the main reservoir.20 Only 8.52% of the current study participants were unaware of monkeys and rodents being the reservoir.
As of 23 Nov 2022 CDC has reported a total of 80,850 cases in 110 location around the word20. A 35 year old man who arrived in Kerala from Middle East was the first case reported from India and the WHO South-East Asia Region.21 Majority (75.58%) of the study participants were aware of the fact. Mode of transmission broadly classified as 1. Animal to human transmission/primary transmission- contact with blood/body fluids, contact with cutaneous/mucosal lesions, bites and scratches, cooking and consumption of infected animals; 2. Human to human transmission/secondary transmission- Direct contact with cutaneous lesions, close contact with recently contaminated object or surfaces, close contact, respiratory droplets.22 Majority (69.7%) of the participants knew the modes of transmission while 30.29 % had some doubt in one or the other documented mode of transmission.
WHO says that the incubation period (interval from infection to onset of symptoms) of monkeypox is usually from 6 to 13 days but can range from 5 to 21 days which 64.41% of the participants correctly answered.23 The course of infection in monkeypox traverse two phases; first being the invasion period (day 1 to day 5) and second by skin eruption period. Invasive period is characterised by fever, headache, chills, myalgia, sore throat and lymphadenopathy. One distinguishing feature of monkeypox is lymphadenopathy usually occurring 1-3 days after the onset of fever that differentiates it from chickenpox, smallpox and measles. The skin eruptions are usually seen from 1-3 days of fever which go through macular, papular, vesicular, and pustular phases.19 In the present study quite low percentage (43.52%) identified all the common sign and symptoms, however most (84.41%) of them were able to tell the correct sequence of progression of rash through different phases. 34.7% of participants correctly identified the majority of commonly occurring complications of monkeypox can include secondary infections, bronchopneumonia, sepsis, encephalitis, and infection of the cornea with ensuing loss of vision.23 Recommended specimen are skin lesion materials like exudates, lesion crusts or swabs from lesion surface20 and a staggering 90.89% of the respondents knew the fact but lacked in knowledge that two swabs from each lesion, preferably from different locations on the body or from lesions that differ in appearance needs to be collected as only 33.52% answered that correctly.20 It was seen that awareness was lacking in knowing the infectivity period of a case of monkeypox which is until the crusts fall off and new skin has formed.20 Participants had a good knowledge of the personal protective equipment to be used when caring for a patient with suspected or confirmed monkeypox or collecting specimens. CDC recommends Gown, Gloves, Eye protection (i.e., goggles or a face shield that covers the front and sides of the face), NIOSH-approved particulate respirator equipped with N95 filters or higher to be worn when entering the patients room.20 However, proper knowledge in infection prevention and control precautions for monkeypox were lacking quite significantly.
When questions regarding attitude and apprehension towards monkeypox was asked majority were unconcerned (63.52%) or very unconcerned (17.05%) about getting monkeypox disease. The reason could be that very few cases (17) of monkeypox has been reported till now with only one death20 which is very less as compared to Covid-19 cases. But the opinion was divided on the question whether Monkeypox outbreak can become as severe as COVID-19 pandemic with neither agreed nor disagreed getting the highest percentage (34.7%). However, a very high percentage agreed that we are still not prepared to tackle monkeypox virus.
Healthcare workers are expected have good knowledge as tend to be involved in publications, read scientific publications, and equip themselves with better knowledge and skills it was found in cases of non-endemic diseases like monkeypox there can be lacunae in the knowledge. Raising awareness, encouraging less risky behaviour and communicating the risk associated with the disease throughout the country particularly areas of high international air travel and areas where recently cases have been recorded is a crucial aspect in controlling or preventing monkeypox spread. Non endemic countries like India should be prepared for outbreaks from exotic pathogens and should device proper surveillance channels and data collection. Enhancing the awareness of health-care workers and even general public should be the first step in preparing for such outbreaks. Knowledge of health care professionals can be amplified by conducting regular seminars, webinars, CMEs on priority basis when such outbreaks are suspected to occur in the country. A multifaceted proactive approach is thus required to fill the gaps in the knowledge of a particular disease which is of utmost importance to fight and control such outbreaks.
The research study has some limitations like being a single centre study and small sample size it soes not reflects the knowledge of whole of India. However, we included budding physicians i.e. medical undergraduates and also nursing staff that play an important role in sample collection, isolation and patient care in India.
Overall knowledge about the human monkeypox virus and disease was underwhelming among the medical students and nursing staff. They can be a vital source of dissemination of knowledge to the general population. In this era of emerging threats, to fill the knowledge gaps of the health care professionals’ strategies like continuing medical education, webinars, seminars, and workshops primarily focussing on better clinical, prevention and control practices should be conducted frequently. More emphasis should be paid on non-endemic, emerging and remerging diseases in the medical and its allied sciences curriculum so that they are prepared to tackle these outbreaks, epidemics and pandemics. Similarly, awareness through outreach programmes, electronic and print media should be spread to enhance the knowledge and reduce the apprehensions of the general population.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
FK, MMH conceptualized the study. MMH, SA performed data curation. FK, SA, MMS applied methodology. SA investigated the study. MMH performed software analysis. FK, SA, AS wrote the manuscript. AS reviewed and edited the manuscript. MSS performed supervision. All authors read and approved the final manuscript for publication.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript.
ETHICS STATEMENT
This article does not contain any studies with human participants or animals performed by any of the authors.
- Ladnyj ID, Ziegler P, Kima E. A human infection caused by monkeypox virus in Basankusu Territory, Democratic Republic of the Congo. Bull World Health Organ. 1972;46(5):593-597.
- WHO recommends new name for monkeypox disease. https://www.who.int/news/item/28-11-2022-who-recommends-new-name-for-monkeypox-disease. Accessed November 30, 2022.
- Centers for Disease Control and Prevention (CDC). Human monkeypox — Kasai Oriental, Democratic Republic of Congo, February 1996-October 1997. MMWR Morb Mortal Wkly Rep. 1997;46(49):1168-1171.
- Durski KN. Emergence of Monkeypox – West and Central Africa, 1970-2017. MMWR Morb Mortal Wkly Rep. 2018;67(10):306-310.
Crossref - Vaughan A, Aarons E, Astbury J, et al. Two cases of monkeypox imported to the United Kingdom, September 2018. Euro Surveill. 2018;23(38):1800509.
Crossref - Vaughan A, Aarons E, Astbury J, et al. Human-to-Human Transmission of Monkeypox Virus, United Kingdom, October 2018. Emerg Infect Dis. 2020;26(4):782-785.
Crossref - Anderson MG, Frenkel LD, Homann S, Guffey J. A case of severe monkeypox virus disease in an American child: emerging infections and changing professional values. Pediatr Infect Dis J. 2003;22(12):1093-1096.
Crossref - Sejvar JJ, Chowdary Y, Schomogyi M, et al. Human monkeypox infection: a family cluster in the midwestern United States. J Infect Dis. 2004;190(10):1833-1840.
Crossref - Learned LA, Reynolds MG, Wassa DW, et al. Extended interhuman transmission of monkeypox in a hospital community in the Republic of the Congo, 2003. Am J Trop Med Hyg. 2005;73(2):428-434.
Crossref - Sklenovska N, Van Ranst M. Emergence of Monkeypox as the Most Important Orthopoxvirus Infection in Humans. Front Public Health. 2018;6:241.
Crossref - Multi-country monkeypox outbreak in non-endemic countries. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON385. Accessed November 29, 2022.
- Harapan H, Setiawan AM, Yufika A, et al. Knowledge of human monkeypox viral infection among general practitioners: a cross-sectional study in Indonesia. Pathog Glob Health. 2020;114(2):68-75.
Crossref - Ricco M, Ferraro P, Camisa V, et al. When a Neglected Tropical Disease Goes Global: Knowledge, Attitudes and Practices of Italian Physicians towards Monkeypox, Preliminary Results. Trop Med Infect Dis. 2022;7(7):135.
Crossref - Bates BR, Grijalva MJ. Knowledge, attitudes, and practices towards monkeypox during the 2022 outbreak: An online cross-sectional survey among clinicians in Ohio, USA. J Infect Public Health. 2022;15(12):1459-1465.
Crossref - Alshahrani NZ, Alzahrani F, Alarifi AM, et al. Assessment of Knowledge of Monkeypox Viral Infection among the General Population in Saudi Arabia. Pathog Basel Switz. 2022;11(8):904.
Crossref - Jairoun AA, Al-Hemyari SS, Abdulla NM, et al. Awareness and preparedness of human monkeypox outbreak among university student: Time to worry or one to ignore? J Infect Public Health. 2022;15(10):1065-1071.
Crossref - Di Giulio DB, Eckburg PB. Human monkeypox: an emerging zoonosis. Lancet Infect Dis. 2004;4(1):15-25.
Crossref - Bunge EM, Hoet B, Chen L, et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl Trop Dis. 2022;16(2):e0010141.
Crossref - Harapan H, Ophinni Y, Megawati D, et al. Monkeypox: A Comprehensive Review. Viruses. 2022;14(10):2155.
Crossref - CDC. Monkeypox in the U.S. Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/poxvirus/monkeypox/veterinarian/monkeypox-in-animals.html. Accessed November 27, 2022.
- Sah R, Mohanty A, Siddiq A, et al. Monkeypox reported in India – South East Asia Region: Health and economic challenges. Lancet Reg Health – Southeast Asia. 2022;4.
Crossref - Kaler J, Hussain A, Flores G, Kheiri S, Desrosiers D. Monkeypox: A Comprehensive Review of Transmission, Pathogenesis, and Manifestation. Cureus. 14(7):e26531.
Crossref - Monkeypox. https://www.who.int/news-room/fact-sheets/detail/monkeypox. Accessed November 27, 2022.
© The Author(s) 2022. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.