ISSN: 0973-7510
E-ISSN: 2581-690X
The interactions between pathogens during infection and the impact of these interactions on drug effectiveness are poorly understood, making polymicrobial infections challenging to treat. During an infection, cross-interactions between bacteria and fungi can strengthen virulence mechanisms and affect how the disease develops. The purpose of this study is to determine how Pseudomonas aeruginosa interacts with Candida glabrata, Candida albicans, Candida krusei, Candida parapsilosis, and Candida tropicalis in the development of polymicrobial biofilms. Pseudomonas aeruginosa, Candida albicans, Candida krusei, Candida parapsilosis, Candida glabrata, and Candida tropicalis isolates were used in this experimental investigation. After preparing a 0.5 Mc Farland suspension of each isolate, the gold standard for measuring biofilm was applied: the Tissue Plate Culture (TCP) method. After that, an ELISA reader with a wavelength of 595 nm was used to measure the optical density (OD) of the biofilm. SPSS 26.0 was then used for statistical analysis to compare the OD values between Pseudomonas aeruginosa that had not been exposed to Candida and those that had. Pseudomonas aeruginosa and Candida are found to interact synergistically if there is an increase in OD, and antagonistic interaction is discovered if there is a decrease in OD. In comparison to the group that was not exposed to Candida, Pseudomonas aeruginosa exposed to Candida albicans, Candida krusei, Candida parapsilosis, Candida glabrata, and Candida tropicalis showed an increase in the OD value of biofilm. Pseudomonas aeruginosa and Candida albicans, Candida glabrata, Candida krusei, Candida parapsilosis, and Candida tropicalis interact synergistically.
Pseudomonas aeruginosa, Candida albicans, Candida glabrata, Candida krusei, Candida parapsilosis, Candida tropicalis, Biofilm, Polymicrobial
Treatment for polymicrobial infections is challenging because the pathogens interactions during infection and how these interactions impact drug efficacy are poorly understood.1 Two opportunistic pathogens that are commonly found in burn wounds and the lungs of patients with cystic fibrosis (CF) and those on mechanical ventilation are Candida albicans and Pseudomonas aeruginosa.2 Fungi and bacteria coexist in a variety of settings, most notably in biofilms, where linked species communicate with one another via distinct signaling pathways. Infections caused by mixed-species biofilms are significantly more difficult to treat than single-species infections, necessitating complex multi-drug treatment strategies.3
One of the key virulence factors in the pathophysiology of an infection with Pseudomonas aeruginosa is the production of biofilm. These pathogens can adhere to a variety of surfaces thanks to biofilms, which shield them from the immune system and different environmental factors. Antibiotic resistance is common as a result of these species interactions.4 The majority of fungus-related infections in humans are caused by species of Candida. The most frequent causes of drug-resistant opportunistic infections like Candida albicans, Candida glabrata, Candida tropicalis, Candida parapsilosis, and Candida krusei, which pose a risk to international public health, are the members of this genus.5
Biofilm formation can determine the state of bacterial persistence in addition to contributing to antibiotic resistance. Biofilm formation is affected by inter-kingdom coinfection, either in an antagonistic or synergistic way.6 During an infection, the interactions among bacteria, fungi, and the immune system can enhance or suppress virulence mechanisms and impact the course of the disease. Pseudomonas aeruginosa and Candida albicans are bacteria and fungi that cause multibacterial infections in many parts of the body, including mucosal tissues like the lungs. Pseudomonas aeruginosa and Candida albicans interact in vitro in a two-way manner that is primarily antagonistic. Their interactions in vivo remain largely unclear, particularly with regard to the host’s reaction to mid-level infections.7
Two opportunistic pathogens, Pseudomonas aeruginosa and Candida albicans, are frequently isolated together through infection, particularly in mucosal tissues like the lungs. This pair of microorganisms is a great example of how little is known about interkingdom interactions, especially in the context of co-infection. According to some studies, bacteria in biofilms can have minimum inhibitory concentrations (MICs) that are 10–10,000 times greater than those of planktonic cells. Therefore, research on the interaction of biofilm formation is crucial, particularly with regard to polymicrobial species.8
Clinically relevant species like Candida albicans and Pseudomonas aeruginosa may interact microbiologically to produce virulence factors that could endanger the host. Using a variety of quorum sensing molecules and phenazines, some of which can be induced in the presence of quorum Pseudomonas aeruginosa inhibits the growth of Candida albicans mycelium when grown in vitro. The discovery that genotypes can differ in their interactions for example, Pseudomonas aeruginosa interacts differently with fungal cells of different morphologies and species when they compete for nutrients and that the environment can affect these interactions led to an increase in the complexity of interactions.9 Psl biofilms were primarily induced on lung cell surfaces by Pseudomonas aeruginosa and Candida albicans in mice that had acute pneumonia. Pseudomonas aeruginosa does not produce a biofilm as large as this one.10
The majority of research has been done to examine the interactions between Pseudomonas aeruginosa and Candida albicans; however, little is known about the interactions between Pseudomonas aeruginosa and other Candida species. A study showed that there are mutually suppressive interactions between Pseudomonas aeruginosa and five non-albicans Candida species, they are: Candida glabrata, C. tropicalis, C. parapsilosis, C. dubliniensis and Candida krusei in an in vitro double biofilm model.11
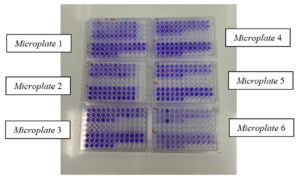
Six isolates of Pseudomonas aeruginosa, six isolates of Candida albicans, six isolates of Candida krusei, six isolates of Candida parapsilosis, six isolates of Candida glabrata, and six isolates of Candida tropicalis that formed the biofilm were obtained from the Clinical Microbiology laboratory at RSUD Dr. Soetomo Surabaya, Indonesia. This was an experimental study. Consecutive sampling was used to gather research samples in order to meet the target number of samples required. The creation of biofilms can be tested using a variety of techniques. The three most effective techniques for identifying biofilm are the Tube Method (TM), Congo Red Agar, and Tissue Culture Plate (TCP).12 The gold standard for measuring biofilm formation was used in this study: isolates of Pseudomonas aeruginosa, Candida albicans, Candida glabrata, Candida krusei, Candida parapsilosis, and Candida tropicalis were subcultured and incubated at 35°C for 24 hours. This procedure is known as the Tissue Culture Plate (TCP) method. In BHI+5% sucrose media, 0.5 McFarland was then suspended and added to a microtiter plate (Figure 1).13
Next, each isolate of Psuedomonas aeruginosa was exposed to each isolate of Candida albicans, Candida glabrata, Candida krusei, Candida parapsilosis, and Candida tropicalis in order to determine the polymicrobial interactions that took place. Following a 24-hour incubation period, the medium was extracted, followed by three PBS washes, methanol fixation, and crystal violet staining. Using an ELISA reader, the density of the biofilm that had formed was determined. Pseudomonas aeruginosa and Candida albicans, Candida glabrata, Candida krusei, Candida parapsilosis, and Candida tropicalis interact polymicrobially. The optical density results from the ELISA reader produced 216 data, which were processed with SPSS 26.0 to compare with Pseudomonas aeruginosa without exposure (Figure 2). An antagonistic relationship results from a decrease in optical density, whereas a synergistic interaction arises from an increase in optical density.
Six isolates of Pseudomonas aeruginosa were obtained and coded as Pa 1, Pa 2, Pa 3, Pa 4, Pa 5, and Pa 6 after the optical density measurement was completed. These isolates formed biofilms with the categories of 5 strong biofilm formation and 1 moderate biofilm formation. Six Candida albicans isolates were identified and coded as Ca1, Ca2, Ca3, Ca4, Ca5, and Ca 6 with the strong biofilm formation category; correspondingly, six Candida glabrata isolates that formed biofilms were identified and coded as Cg1, Cg2, Cg3, Cg4, Cg5, and Cg with the strong biofilm formation category, The following six isolates were found to be forming biofilms: six isolates of Candida krusei were found and coded as Ck 1, Ck 2, Ck 3, Ck 4, Ck 5, and Ck 6 with the category of strong biofilm formation; six isolates of Candida parapsilosis were found and coded as Cp 1, Cp 2, Cp 3, Cp 4, Cp 5 and Cp 6 with the category of strong biofilm formation; and six isolates of Candida tropicalis were found and coded as Ct 1, Ct2, Ct 3, Ct 4, Ct 5, and Ct 6 with the category of strong biofilm formation (Table 1).
Table (1):
The categories of isolate sample from the measurement of optical density
No. |
Isolate codes |
Isolate names |
OD |
Categories |
|---|---|---|---|---|
1 |
Pa 1 |
Pseudomonas aeruginosa |
0.279 |
Strong biofilm formation |
2 |
Pa 2 |
Pseudomonas aeruginosa |
0.485 |
Strong biofilm formation |
3 |
Pa 3 |
Pseudomonas aeruginosa |
0.255 |
Strong biofilm formation |
4 |
Pa 4 |
Pseudomonas aeruginosa |
0.25 |
Strong biofilm formation |
5 |
Pa 5 |
Pseudomonas aeruginosa |
0.271 |
Strong biofilm formation |
6 |
Pa 6 |
Pseudomonas aeruginosa |
0.213 |
Moderate biofilm formation |
7 |
Ca 1 |
Candida albicans |
0.52 |
Strong biofilm formation |
8 |
Ca 2 |
Candida albicans |
0.793 |
Strong biofilm formation |
9 |
Ca 3 |
Candida albicans |
0.677 |
Strong biofilm formation |
10 |
Ca 4 |
Candida albicans |
0.468 |
Strong biofilm formation |
11 |
Ca 5 |
Candida albicans |
0.542 |
Strong biofilm formation |
12 |
Ca 6 |
Candida albicans |
0.415 |
Strong biofilm formation |
13 |
Cg 1 |
Candida glabrata |
0.886 |
Strong biofilm formation |
14 |
Cg 2 |
Candida glabrata |
0.942 |
Strong biofilm formation |
15 |
Cg 3 |
Candida glabrata |
0.655 |
Strong biofilm formation |
16 |
Cg 4 |
Candida glabrata |
0.452 |
Strong biofilm formation |
17 |
Cg 5 |
Candida glabrata |
0.758 |
Strong biofilm formation |
18 |
Cg 6 |
Candida glabrata |
0.825 |
Strong biofilm formation |
19 |
Ck 1 |
Candida krusei |
0.492 |
Strong biofilm formation |
20 |
Ck 2 |
Candida krusei |
0.524 |
Strong biofilm formation |
21 |
Ck 3 |
Candida krusei |
1.952 |
Strong biofilm formation |
22 |
Ck 4 |
Candida krusei |
1.696 |
Strong biofilm formation |
23 |
Ck 5 |
Candida krusei |
0.356 |
Strong biofilm formation |
24 |
Ck 6 |
Candida krusei |
0.422 |
Strong biofilm formation |
25 |
Cp 1 |
Candida parapsilosis |
0.971 |
Strong biofilm formation |
26 |
Cp 2 |
Candida parapsilosis |
1.318 |
Strong biofilm formation |
27 |
Cp 3 |
Candida parapsilosis |
0.725 |
Strong biofilm formation |
28 |
Cp 4 |
Candida parapsilosis |
0.52 |
Strong biofilm formation |
29 |
Cp 5 |
Candida parapsilosis |
0.707 |
Strong biofilm formation |
30 |
Cp 6 |
Candida parapsilosis |
1.005 |
Strong biofilm formation |
31 |
Ct 1 |
Candida tropicalis |
0.589 |
Strong biofilm formation |
32 |
Ct 2 |
Candida tropicalis |
0.67 |
Strong biofilm formation |
33 |
Ct 3 |
Candida tropicalis |
0.694 |
Strong biofilm formation |
34 |
Ct 4 |
Candida tropicalis |
1.368 |
Strong biofilm formation |
35 |
Ct 5 |
Candida tropicalis |
0.637 |
Strong biofilm formation |
36 |
Ct 6 |
Candida tropicalis |
0.533 |
Strong biofilm formation |
The categorization of biofilm formation was obtained based on the formula:
- OD isolate ≤ Optical Density cutoff value (ODC) (0) no biofilm forming,
- ODC < OD Isolate ≤ 2 x ODC (+ or 1) weak biofilm forming,
- 2x ODC < OD Isolate ≤ 4 x ODC (++ or 2) moderate biofilm forming,
- 4 x ODC < OD Isolate (+++ or 3) high/strong biofilm forming10
The computation results indicate that the average negative control (Odav) = 0.043 with a Standard Deviation of 0.005, where ODC was the average negative control/Optical density average value (Odav)+3x Standard Deviation (SD) measured at 595 nm.13 ODC= Odav+SD=0.043+(3×0.005) = 0.058= 0.06 was calculated using this formula.
Based on the categorization in this study, it can be interpreted that:
- No biofilm forming: OD<0,06
- weak biofilm forming: OD= 0,06 – 0,12
- moderate biofilm forming: OD= 0,12 – 0,24
- strong biofilm forming: OD > 0,24
The SPSS 26.0 Kruskal Wallis test application was used to process the data after the OD of the biofilm result was obtained. Next, the following OD comparison was obtained between Pseudomonas aeruginosa in the absence of exposure and in the presence of Candida albicans, Candida glabrata, Candida krusei, Candida parapsilosis, and Candida tropicalis:
Pseudomonas aeruginosa and Candida tropicalis had the highest interaction value (145.25), followed by Pseudomonas aeruginosa and Candida albicans (135.90), Pseudomonas aeruginosa and Candida krusei (127.35), Pseudomonas aeruginosa and Candida parapsilosis (107.40), and Pseudomonas aeruginosa and Candida glabrata (102.28). These three combinations were determined using Post hoc tests (Table 2).
Table (2):
The difference of the optical density of single P. aeruginosa and with the exposure to Candida
| OD single | Pseudomonas aeruginosa+ Candida | Interpretation | Nature of Interaction | |
|---|---|---|---|---|
| Pseudomonas aeruginosa | ||||
| C. albicans | 0,292 | 0,915 | Increased | Synergistic |
| C. glabrata | 0,292 | 0,636 | Increased | Synergistic |
| C. krusei | 0,292 | 0,829 | Increased | Synergistic |
| C. parapsilosis | 0,292 | 0,664 | Increased | Synergistic |
| C. tropicalis | 0,292 | 1,167 | Increased | Synergistic |
Out of the 36 isolates in this study, 35 showed strong biofilm formation, and 1 showed moderate biofilm formation. It demonstrates that the formation of biofilms is a crucial virulence factor14 for both Pseudomonas aeruginosa and the species of Candida. Because of biofilms, these infections can adhere to a variety of surfaces, shielding them from the host immune system and various environmental factors such as dehydration and violence, as well as natural killer cells, phagocytes, complement, and ROS-mediated damage. These interspecies interactions are typically more resistant to antimicrobial agents than other microorganisms.8
Together, the fungi and bacteria can be found in a range of settings, but biofilms are particularly common. In these structures, the attached species communicate with one another via a variety of signaling pathways. Due to the formation of biofilms, interspecies interactions can influence drug intolerance, virulence factors, and the outcome of polymicrobial infections.15 Pseudomonas aeruginosa caused pneumonia may be predisposed to by Candida albicans colonization, according to a clinical study done on ventilated patients.1
According to this study, Pseudomonas aeruginosa exposed to Candida albicans, Candida glabrata, Candida krusei, Candida parapsilosis, and Candida tropicalis showed an increase in OD. One significant effect of these phenotypic modifications is modified antibiotic tolerance. Antimicrobial concentrations needed to destroy biofilms are many times greater than those needed to treat planktonic bacterial infections, which are more common. As a result, for biofilm-associated infections, microbiological indices of antimicrobial susceptibility like minimal inhibitory concentration (MIC) that direct the selection of treatment for common infections are unreliable. Furthermore, the patient’s symptoms are frequently exacerbated by an inflammatory response, as the immune system is unable to effectively eradicate the infection. Lastly, live bacteria in the form of persistence or small colony variants can also be found within the biofilm structure. Consequently, biofilm-related infections are thought to be challenging to treat. In certain cases, such as infections related to catheters, patients’ biofilms can be effectively treated by removing the infected foreign body; however, this is not always the case, necessitating prolonged use of high doses of antibiotics and frequent surgery.15
In this study, it was found that there was a difference in OD between Pseudomonas aeruginosa and the OD of Pseudomonas aeruginosa with exposure to Candida albicans, where there was an increase in OD which indicated a synergistic interaction. Candida albicans produces ethanol due to the induction by Phenazine from Pseudomonas aeruginosa and the ethanol which stimulates adhesion and biofilm formation of Pseudomonas aeruginosa. There is a positive feedback mechanism where Candida albicans ethanol production can increase 5-methyl-phenazine-1-carboxylic acid (5-MPCA) production in Pseudomonas aeruginosa and increase biofilm formation. Then, 5-MPCA stimulates ethanol production in Candida albicans.16
Similar findings were also found in a study conducted in 2021 by Kasetty et al., which showed that Pseudomonas aeruginosa biofilms containing Candida albicans had higher OD levels than Pseudomonas aeruginosa biofilms alone.14 It also bore similarities to Phuengmaung’s research from 2022, which discovered that prominent interkingdom biofilms with more severe infections were induced by Pseudomonas and Candida in the lungs of patients suffering from cystic fibrosis and ventilation-associated pneumonia (VAP). Compared to Pseudomonas and single Candida,9 the biofilm production between Pseudomonas added with Candida was more increased. However, this is not the same as the results of research by Fourie et al. in 2019, which showed a decrease in OD indicating an antagonistic interaction.8
Pseudomonas aeruginosa and Candida albicans both produce more biofilms than a single Pseudomonas aeruginosa, most likely as a result of their distinct biofilm properties and the significance of multiple genes for Pseudomonas biofilm production, especially for biofilms from the polysaccharide synthesis locus (Psl) as opposed to the alginate-mediated pathway. Pseudomonas virulence factors that were significant were the genes (alginate, psl, and pel) that produce the pseudomonas biofilm. Alginate was a negatively charged acetylated polymer that was used to increase reactive oxygen species in host cells and inhibit phagocytosis. It contained nonrepetitive b-1,4-linked L -guluronic and D -mannuronic acids. Psl is a neutral branched pentasaccharide that mediates attachment to lung epithelial cells, promoting pro-inflammatory responses and host cell damage. It has a 1:1:3 ratio of D-glucose, D-rhamnose, and D-mannose. Pel, on the other hand, was a positively charged polysaccharide that stabilized the biofilm structure by acetylating one to four glycosidic branches from N-acetyl galactosamine and N-acetylglucosamine. We can therefore conclude that the psl gene plays a role in the increase in OD in mixed biofilms.10
A number of publications have demonstrated that Pseudomonas aeruginosa and Candida albicans interact antagonistically. One such publication, by Fourie et al., demonstrates that quorum sensing molecules and phenazines mediate antagonistic interactions between Pseudomonas aeruginosa and Candida albicans. However, the presence of biofilm heterogeneity between in vitro and in vivo studies can lead to different results.9
Additional research demonstrates that interactions between the fungus Candida albicans and the bacteria Pseudomonas aeruginosa led to more severe infections in the human host. Pseudomonas aeruginosa’s production of biofilms is linked to more challenging-to-treat infections. Pseudomonas aeruginosa is stimulated by ethanol to colonize respiratory tract cells and plastic surfaces. The fungus also produces ethanol, which modifies the toxic spectrum of Pseudomonas aeruginosa’s phenazine, which is linked to worsening lung function in cystic fibrosis patients.8 A positive feedback loop between Candida albicans and Pseudomonas aeruginosa occurs as a result of phenazine’s interaction with Candida albicans to promote ethanol production, which exacerbates the disease. When exposed to low concentrations of Candida albicans, phenazine increased the production of fermentation products like ethanol by three to five times. However, at high concentrations, phenazine is toxic to Candida albicans.17
In this investigation, it was discovered that Pseudomonas aeruginosa’s OD differed from that of the bacteria when exposed to Candida glabrata, with the latter exhibiting an increase in OD that suggested a synergistic interaction. One of the typical flora commonly found in the gastrointestinal tract, vagina, and oral cavity is Candida glabrata, an organism that is widely distributed. But it can also be harmful and lead to severe infections, which are more likely to happen in patients with compromised immune systems.18 One of Candida glabrata’s worrisome virulence factors is its capacity to form biofilms.19 These days, the relationship between Pseudomonas aeruginosa and Candida glabrata in biofilm formation is still largely unexplored in polymicrobial research. Only two published studies have indicated that Pseudomonas aeruginosa and Candida glabrata have an antagonistic interaction. These studies also demonstrate a decrease in the OD of the mixture of Pseudomonas aeruginosa and Candida glabrata when compared to the OD of Pseudomonas aeruginosa alone.9,20
Phenazines are among the molecules produced by Pseudomonas that induce ethanol from Candida. Candida glabrata also produces ethanol, and this ethanol can help Pseudomonas through the psl operon facilitate its extracellular matrix as a positive feedback to adapt to the microenvironment and increase the formation of biofilm.17 As a result, when Pseudomonas aeruginosa is exposed with Candida glabrata, the amount of OD increases. It has been demonstrated by a study that, in contrast to the other three species, C. glabrata can form biofilms in low glucose concentrations and under unfavorable nutritional conditions. This is most likely because C. glabrata can acclimate to these circumstances and selectively colonize certain human tissues.21
The results of this study showed that Pseudomonas aeruginosa and those exposed to Candida krusei differed in their OD values, with the latter showing an increase in OD that suggested a synergistic interaction. One of Candida krusei’s virulence factors is its capacity to form biofilms.22 Pseudomonas aeruginosa can stimulate Candida krusei’s ethanol production, which thickens Pseudomonas aeruginosa’s extracellular matrix and raises OD. This mechanism is similar to that of Candida albicans and Candida glabrata.17
Interactions between various species alter the host response, the effectiveness of antibiotics, the pathogenesis and virulence of the bacteria, and generally make infections worse and make them more resistant to traditional treatment.23 Polymicrobial research on the role of Candida krusei and Pseudomonas aeruginosa in biofilm formation is still lacking at this time. Only one published study, which demonstrated a drop in the optical density (OD) of the mixture of Pseudomonas aeruginosa and Candida krusei relative to the OD of single Pseudomonas aeruginosa, suggested that there was an antagonistic interaction between the two species.8
Similar to other Candida, Pseudomonas aeruginosa can stimulate ethanol production in Candida parapsilosis which causes thickening of the extracellular matrix in Pseudomonas aeruginosa15 so that it causes an increase in OD. In this study, it was found that there was a difference in OD between Pseudomonas aeruginosa and the OD of Pseudomonas aeruginosa exposed to Candida parapsilosis, in which there was an increase in OD indicating a synergistic interaction.
Candida parapsilosis forms thinner, less complex biofilms than Candida albicans. On implanted plastic medical devices, however, C. parapsilosis biofilms continue to be a major source of infection.24 Polymicrobial research on the role of Candida parapsilosis and Pseudomonas aeruginosa in biofilm formation is still lacking. The antagonistic interaction between Pseudomonas aeruginosa and Candida parapsilosis, indicated by a decrease in the optical density (OD) of the mixture of Pseudomonas aeruginosa and Candida parapsilosis relative to the OD of single Pseudomonas aeruginosa, has only been reported in two published studies.9,20
The results of this investigation showed that Pseudomonas aeruginosa and those exposed to Candida tropicalis differed in terms of their OD, with the former showing an increase in OD that suggested a synergistic interaction. Like other Candida, Pseudomonas aeruginosa can induce Candida tropicalis to produce ethanol, which thickens Pseudomonas aeruginosa’s extracellular matrix and raises the organism’s optical density (OD).17 In most studies, Candida tropicalis outperforms Candida albicans in its ability to produce biofilm.25
In a previous investigation of the antagonistic relationship between Candida tropicalis and Pseudomonas aeruginosa, Wahyuning et al.26 discovered that Pseudomonas aeruginosa inhibited the formation of biofilms in Candida tropicalis. Pseudomonas aeruginosa and Candida tropicalis biofilm former isolates were also used in this investigation. Because the strain used in this study is capable of killing C. tropicalis hyphae and biofilms, which are caused by phenazine compounds that compromise the integrity of cell walls, antagonistic relationships arise in P. aeruginosa mixed species. This work, however, is in line with earlier in vitro biofilm studies that demonstrated P. aeruginosa can inhibit the growth of Candida biofilms that are not albicans, such as C. tropicalis.
This is due to the fact that Gram negative bacteria contain N-acyl homoserine lactone (AHL) and that these two microbes have the ability to release quorum sensing molecules. In the meantime, AHL in P. aeruginosa can be decreased in vitro to prevent Candida spp. biofilms.25 Comparable to studies by Fourie et al. and Bandara et al. that reported an antagonistic interaction between Pseudomonas aeruginosa and Candida tropicalis and demonstrated a drop in the optical density (OD) of a mixture of the two species relative to the OD of Pseudomonas aeruginosa alone.9,20 Pseudomonas aeruginosa and Candida spp. both form biofilms, according to a study by Bandara. Each isolate used in the study was the ATCC strain, which can result in various interactions between Pseudomonas aeruginosa and Candida spp.20
Pseudomonas aeruginosa exposed to Candida albicans, Candida glabrata, Candida krusei, Candida parapsilosis, and Candida tropicalis showed an increase in the OD value of the biofilm compared to the group that was not exposed to Candida. This suggests that Pseudomonas aeruginosa and Candida albicans, Candida glabrata, Candida krusei, Candida parapsilosis, and Candida tropicalis work synergistically.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript.
ETHICS STATEMENT
This study was approved by the Health Research Ethics Committee at Dr. Soetomo Regional General Hospital Surabaya number 1344/LOE/301.4.2/VI/2023.
- Hattab S, Dagher AM, Wheeler RT. Pseudomonas Synergizes with Fluconazole against Candida during treatment of polymicrobial infection. Infect Immun. 2022;90(4):e0062621.
Crossref - Behzadi P, Barath Z, Gajdacs M. It’s not easy being green: a narrative review on the microbiology, virulence and therapeutic prospects of multidrug-resistant Pseudomonas aeruginosa. Antibiotics. 2021;10(1):42.
Crossref - Ponde NO, Lortal L, Ramage G, Naglik JR, Richardson JP. Candida albicans biofilms and polymicrobial interaction. Crit Rev Microbiol. 2021;47(1):91-111.
Crossref - Tuon FF, Dantas RL, Suss PH, Ribeiro VS. Pathogenesis of the Pseudomonas aeruginosa biofilm: a review. Pathogens. 2022;11(3):300.
Crossref - Lopes JP, Lionakis MS. Pathogenesis and virulence of Candida albicans. Virulence. 2022;13(1):89-121.
Crossref - Dianty R. Interaksi Candida Albicans dan bakteri batang Gram negatif (Pseudomonas aeruginosa dan Acinetobacter baumannii) pada pembentukan biofilm. Universitas Airlangga. 2020. https://repository.unair.ac.id/104023/. Accessed August 20, 2022.
- Bergeron AC, Seman BG, Hammond JH, Archambault LS, Hogan DA, Wheeler RT. Candida albicans and Pseudomonas aeruginosa interact to enhance virulence of mucosal infection in Transparent Zebrafish. Infect Immun. 2017;85(11):e00475-17.
Crossref - Grainha T, Jorge P, Alves D, Lopes SP, Pereira MO. Unraveling Pseudomonas aeruginosa and Candida albicans communication in coinfection scenarios: insights through network analysis. Front Cell Infect Microbiol. 2020;10:550505.
Crossref - Fourie R, Pohl CH. Beyond antagonism: the interaction between Candida Species and Pseudomonas aeruginosa. J Fungi. 2019;5(2):34.
Crossref - Phuengmaung P, Mekjaroen J, Saisorn W, Chatsuan T, Somparn P, Leelahavanichkul A. Rapid synergistic biofilm production of Pseudomonas and Candida on the pulmonary cell surface and in Mice, a possible cause of chronic mixed organismal lung lesions. Int J Mol Sci. 2022;23(16):9202.
Crossref - Syaiful I, Widodo ADW, Endraswari PD, Alimsardjono L, Utomo B, Arfijanto MV. The association between biofilm formation ability and antibiotic resistance phenotype in clinical isolates of Gram negative bacteria: a cross-sectional study. Bali Medical Journal. 2023;12(1):1014-1020.
Crossref - Normanita R. Perbandingan sensitivitas dan spesifisitas metode Congo Red Agar dan Modified Congo Red Agar untuk deteksi produksi biofilm pada isolat klinis Enterococcus Faecalis. Universitas Airlangga. 2019. https://repository.unair. ac.id/96883/. Accessed August 15, 2022
- Swedan S, Shubair Z, Almaytaah A. Synergism of cationic antimicrobial peptide WLBU2 with antibacterial agents against biofilms of multi-drug resistant Acinetobacter baumannii and Klebsiella pneumoniae. Infect Drug Resist. 2019;12:2019-2030.
Crossref - Kassety S, Mould DL, Hogan DA, and Nadell CD. Both Pseudomonas aeruginosa and Candida albicans accumulate greater biomass in dual-species biofilms under flow. mSphere. 2021;6(3):e00416-21.
Crossref - Tamayo JL, Carmora AM. The clinical meaning of biofilm formation ability. Microbiologia Clinica. 2022;40(8):415-417.
Crossref - Chen AI, Dolben EF, Okegbe C, et al. Candida albicans ethanol stimulates Pseudomonas aeruginosa WspR-controlled biofilm formation as part of a cyclic relationship involving phenazines. Plos Pathogen. 2014;10(10):e1004480.
Crossref - Talapko J, Juzbasic M, Matijevic T, et al. Candida albicans the virulence factors and clinical manifestations of infection. J Fungi. 2021;7(2):79.
Crossref - Hassan Y, Chew SY, Than LTL. Candida glabrata: pathogenicity and resistance mechanisms for adaptation and survival. J Fungi. 2021;7(8):667.
Crossref - Bandara HMHN, Yau JYY, Watt RM, Samaranayake LP. Pseudomonas aeruginosa inhibits in-vitro Candida biofilm development. BMC Microbiol. 2010;10:125.
Crossref - Fujarte IS, Romero EL, Lopez GER, et al. Influence of culture media on biofilm formation by Candida species and response of sessile cells to antifungals and oxidative stress. BioMed Res Int. 2015;783639.
Crossref - Barros PP, Rossoni RD, Souza CM, et al. Candida biofilms: an update on developmental mechanisms and therapeutic challenges. Mycopathologia. 2020;185(3):415-424.
Crossref - Qin S, Xiao W, Zhou C, et al. Pseudomonas aeruginosa: pathogenesis, virulence factors, antibiotic resistance, interaction with host, technology advances and emerging therapeutics. Signal Transduct Target Ther. 2022;7(1):199.
Crossref - Cavalheiro M, Teixeira MC. Candida biofilms: threats, challenges and promising strategies. Front Med. 2018;5:28.
Crossref - Gaviria MG, Montes HMM. Current aspects in the biology, pathogeny and treatment of Candida krusei, a neglected fungal pathogen. Infect Drug Resist. 2020;13:1673-1689.
Crossref - Wahyuning D, Widodo ADW, Setiabudi RJ, et al. Biofilm formation by the interaction of fungi (Candida tropicalis) with various bacteria. Journal of Advanced Biotechnology and Experimental Therapeutics. 2022;6(1):84-93.
Crossref
© The Author(s) 2024. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.