ISSN: 0973-7510
E-ISSN: 2581-690X
Hepatitis E virus (HEV) is the most common cause of AVH in developing countries. HEV causes a self-limiting infection that is transmitted mainly through the consumption of contaminated food and water. Our study aimed to find out the seroprevalence of HEV infection. Detected both IgG & IgM antibodies from 100 asymptomatic antenatal women. ELISA (DIA PRO, Italy) was used to detect antibodies. Seropositivity was found in 9% of pregnant women, all might have been exposed to HEV infection previously. It could be unnoticed due to its self-limiting nature. IgG was 5% and IgM was 6%. Both IgM & IgG were detected in two pregnant women. Untreated water was used by the majority of women irrespective of their educational status. Though it is a self-limiting disease, it is necessary to screen for its antibody. Awareness about the modes of transmission & complications needs to be addressed in the community. It is necessary to do further studies for screening for HEV infection as there is a very limited number of studies published from South India.
Hepatitis Virus, Jaundice, Immunoglobulin
Viral hepatitis is a major public health problem in India and Acute Viral Hepatitis (AVH) continues to be present even after improving sanitation, health awareness, and socioeconomic conditions. AVH is one of the most important systemic infections, caused by viruses that are hepatotropic to which man is prone. India is hyperendemic for hepatitis A and E.1 Hepatitis E virus (HEV) is the most common cause of acute viral hepatitis in developing countries, including India, and 20 million human cases are reported around the world every year.
HEV causes a self-limiting infection that is transmitted by the faeco-oral route, mainly through the consumption of contaminated food and water or coming into contact with untreated sewage.2-4 Moreover, blood transfusion is an additionally reported route of transmission of the hepatitis E virus. In India, HEV is mainly caused by genotype 1 (pathogenic only for humans and non-human primates as genotype 2) and zoonotic transmission (genotypes 3 and 4 circulating in several animals around the World) appears to be rare.5-7
Hepatitis E, although it is recognized as a self-limiting disease in developing countries, pregnant women develop more severe symptomatic disease.8 In Pregnant women, the development of fulminant hepatic failure is the major complication of outbreaks caused by genotype.1 The mortality rate can be as high as 30% and usually occurs in the 3rd trimester of pregnancy.9
Rate of HEV seropositivity is not expected to be higher in pregnant women compared to general population, but the disease manifested as severe with poorer prognosis in this specific population.
Hepatitis E infection is infrequent in areas with better sanitation and water supply. Serological evidence of prior exposure to the virus has been found in most areas, with higher seroprevalence rates in regions with lower standards of sanitation and thus higher risk for transmission.10 Considering that Hepatitis E infection can represent a risk in pregnancy, the goal of this study was to survey the seroprevalence of this virus in antenatal women from tertiary care centre in Puducherry (India), in order to investigate our region where there are no previous studies reported.
Aims and Objectives
- To detect the presence of IgM & IgG antibodies against Hepatitis E antigen in antenatal women.
- To analyse the factors associated with the seroprevalence of Hepatitis E antibodies in our region, Puducherry, India.
All serum samples (n=100) were screened for the presence of HEV antibodies (IgM and IgG) by using enzyme-linked immunosorbent assay (ELISA) kits ( DIA.PRO- Italy). The ELISA was performed according to the protocols provided by the manufacturer. Test results were interpreted as ratio of the sample OD 450nm and cut–off value according to the following criteria given by the manufacturer.
“A series of sociodemographic information were also collected to find out the associated factors influencing seroprevalence achieved in the antenatal women involved in the present study. These include socioeconomic status, educational qualification, drinking water quality, sanitation practices, etc. All details were entered in an Excel sheet, and the percentage (% out of total number and positives) was calculated (Table).
A cross-sectional, descriptive study was carried out for a period of two months to determine the seroprevalence of Hepatitis E antibodies in asymptomatic antenatal women from the tertiary care centre, Puducherry (India).
All asymptomatic antenatal women attended outpatient and inpatient departments during the study period. After getting consent from the Institute Ethics Committee, samples were collected from consecutive antenatal women attending out patients and in patient, Obstetrics & Gynaecology department. A total of 100 samples were collected from asymptomatic antenatal women. No repeat sample was collected from the same person. Blood samples were collected along with regular screening tests during the antenatal check-up. And the serum was separated and preserved in a deep freezer (-20°C) before the detection
Blood samples from asymptomatic antenatal women were collected for HEV IgM and IgG detection. The majority of them were in their third trimester of pregnancy. Sample collection has completed within three months period. Blood samples were collected (2ml) from asymptomatic antenatal women along with regular screening tests during the pregnancy check-up. All sera were separated and preserved in a deep freezer (-20°C) until use. No repeat sample was collected from the same person.” Among the antenatal women studied, 59% of them are well educated with graduation and post graduation. Only 3 of them are illiterate. Remaining all have studied upto higher secondary schooling.
The age range of our study subjects is from 19 to 42yrs. Regarding the quality of drinking water, only 21% of them use boiled water. The socioeconomic status of our study group includes middle level. There was no one belonging to low socioeconomic status. In our study, 82% of the antenatal women were from rural areas. The Table shows antibody positivity in relation to some demographic variables.
Table:
Sociodemographic characteristics.
| Variables | Total Number (n=100) | No. Of Positives (n=9) | (%) out of total number | (%) out of total positives | |||
|---|---|---|---|---|---|---|---|
| 1
|
Place of residence | Urban | 18 | 5 | 27.7 | 55.6 | |
| Rural | 82 | 4 | 4.9 | 44.4 | |||
| 2
|
Educational status | Post graduates | 18 | – | |||
| Graduates | 41 | 6 | 14.6 | 66.7 | |||
| Higher secondary | 26 | – | |||||
| Primary school | 12 | 2 | 16.6 | 22.2 | |||
| Illiterate | 03 | 1 | 33.3 | 11.1 | |||
| 3
|
Drinking Water | Untreated water | 79 | 6 | 7.6 | 66.7 | |
| Boiled water | 21 | 3 | 14.2 | 33.3 | |||
| 4
|
Past history of jaundice | Present | 09 | 2 | 22.2 | 22.2 | |
| Absent | 91 | 7 | 7.7 | 77.7 | |||
| 5 | Socioeconomic status | Middle | 100 | 9 | 9 | 100 | |
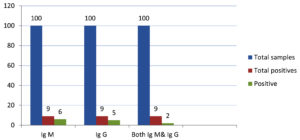
Out of 100, nine (9%) samples were positive for HEV antibodies. In which six (6%) of them were positive for IgM and five (5%) were IgG Positive (Figure). In two samples, equivocal results were noticed for IgM. Similarly, in one sample, IgG was also found to be equivocal. But we could not repeat it after two weeks for confirmation. Two samples were positive for both IgM & IgG.
HEV infection is a major public health concern. Large-scale epidemics and sporadic cases of acute viral hepatitis in developing countries are caused by Hepatitis E Virus. The infection is generally mild and self-limiting. HEV during pregnancy, especially in the third trimester, is a potential risk factor for fulminant hepatic failure and maternal death. Out of 100 antenatal women screened for HEV antibodies, nine ( 9%) of them were found to be positive in our study. All participants are asymptomatic, no signs of liver involvement are noticed. Overall seropositivity is 9%. Totally, six of them were positive for IgM and five for IgG. This type of low positivity was reported by many authors in their studies. In our country, many studies have been done to find out the seroprevalence of HEV infection and some studies specifically targeted pregnant women as they are more vulnerable to this infection. Most of the studies were aimed to detect IgG antibodies. Our study coincides with a previous study performed in Chennai, Tamil Nadu study where a prevalence rate of 14% was reported Sivasangeetha et al.11 This explains that the lifestyle of Chennai people are not much different from our region in relation to their educational status, sanitation practice and the quality of drinking water. A study from France showed a 7.7% prevalence, which is also similar to our finding. None of the HEV IgG positive women reported a history of liver disease.12
A high seropositivity, 33.67% is reported in a study carried out in Delhi, where the investigated population was also represented by asymptomatic women.13 In a study from Bangladesh, out of the 255 asymptomatic pregnant women, 96 (37.6%) tested positive for anti-HEV IgG antibodies.
Higher seroprevalence of anti-HEV IgG (57.4%) was observed among pregnant women of lower middle class compared to the upper middle class (15.1%) by Sultana, G et al. from Bangladesh.14 Higher prevalence was associated with low socioeconomic status, which is considered as one of the risk factors.13 Educational status has no significance observed in our study. Studies show significantly higher prevalence among the urban population than in the rural population. A report from Vellore proved that 19.91% positive in urban population, but only 9.09% seen in the rural population. In our study, the same finding was observed, 27.7% and 4.9% positivity seen among the urban & rural population respectively. “There is an increasing trend in HEV antibody seroprevalence, which was observed in some studies but that result was not significant according to the authors.”
As far as IgM 6% of samples tested were found to be positive. The presence of IgM indicates acute infection, but all participants in our study were asymptomatic. There was no signs of jaundice. Past history of jaundice had given by 9 antenatal mothers. Out of the six positive cases, two of them had jaundice during their school days. There are wide range in seroprevalence reported from national and global studies. A study performed in Nigeria showed 0.4% positive for HEV IgM among pregnant women. Singh et al.15 from “All India Institute of Medical Sciences” (AIIMS), Delhi, studied in symptomatic patients suspected of AVH. A very high positivity (40%) for IgM noticed. In 2003 another study from same centre showed 36.6% positivity for IgM anti-HEV antibodies among suspected antenatal women.16 In both the above mentioned studies, study subjects were suspected patients. So the positivity was high. A study performed at the Red Crescent General Hospital and Saint Elizabeth Hospital, Hyderabad, showed 48.9% of HEV infected pregnant women were having severe complications.17 Our study subjects are asymptomatic women, so we have not aimed to know about the complications. HEV infection during pregnancy, especially in the third trimester, leads to poor fetomaternal outcomes due to fulminant hepatitis.
Anuradha et al.18 reported a high (60%) prevalence of HEV IgM, which is very high compared to our study. In their study they have used Rapid test (ICT) for the detection of IgM. Also majority of participants use open sanitation practice, which is one of the risk factors associated with the HEV prevalence.18
In our study majority of participants are well educated (59%). Previous studies have reported that HEV IgG seropositivity was more common in women who did not complete their higher secondary level of education.14 Our study found that 20% positivity in people who have not completed higher secondary which is little higher (14.6%) than those who have done graduation and post graduation. Study by Bigna et al., from Cameroon, reported seroprevalence of 3.5% in asymptomatic pregnant women.19 Another similar study from China, 6.0% of pregnant women were positive for anti-HEV IgG antibody, 0.3% were anti-HEV IgM antibody positive and 0.3% were positive for both anti-HEV IgG and anti-HEV IgM antibodies, which was well in concordance with our study.20 Mustafa et al.21 in their study reported high prevalence of 40% for IgG antibodies and 6% positive for IgM antibodies, access to healthy food and clean water is almost impossible for study participants. Such conditions provide a great environment for disease.
In our study all participants belong to third trimester. It was reported that prevalence rate is more among pregnant women in third trimester than first and second trimester.14
The reason for these variation in prevalence rate as reported from various part of country could be due to early childhood HEV exposures producing long lasting immunity. Positivity also noted in close contacts of patients in some studies.
Overall seroprevalence was found to be low in our study. As our study group is asymptomatic antenatal women, even this low prevalence rate (9%) can be taken into consideration.
There was no past history of Jaundice or any other symptoms related to HEV infection given by majority of the positive cases. Complications and fatality are most common in pregnant women infected with HEV. It also cause vertical transmission. Though it is a self limitingdisease, it is necessary to screen for its antibody. Awareness about the modes of transmission and complications needs to address in community. So that people can change their life style to prevent this infection. Untreated water was used by majority of women irrespective of their educational status. It is necessary to do further studies for screening HEV infection as there is very limited number of studies published from south India.
Limitations of our study
Sample size is moderate in our study. We could not repeat sample for the results which are equivocal. Liver function tests could not be performed in positive cases.
ACKNOWLEDGMENTS
The authors would like to thank ICMR, Obstetrics and Gynecology Department, Mahatma Gandhi Medical College & Research Institute, Pondicherry, India, for providing their support.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript.
ETHICS STATEMENT
This study was approved by the Institutional Ethics Committee, Sri Balalji Vidyapeeth (Deemed to be University), Mahatma Gandhi Medical College & Research Institute, Puducherry, India, with reference number ICMR Project/08/2019/06.
INFORMED CONSENT
Written informed consent was obtained from the participants before enrolling in the study.
- Gupta E, Agarwala P. Hepatitis E virus infection: An old virus with a new story. Indian J Med Microbiol. 2018;36(3):317.
Crossref - Van der Poel WH. Food and environmental routes of Hepatitis E virus transmission. Curr Opin Virol. 2014;4:91-96.
Crossref - Naik SR, Aggarwal R, Salunke PN, Mehrotra NN. A large waterborne viral hepatitis E epidemic in Kanpur, India. Bull World Health Organ. 1992;70(5):597-604. PMCID: PMC2393368.
- Di Profio F, Melegari I, Palombieri A, et al. High prevalence of hepatitis E virus in raw sewage in Southern Italy. Virus Res. 2019;272:197710.
Crossref - Tripathy AS, Puranik S, Sharma M, Chakraborty S, Devakate UR. Hepatitis E virus seroprevalence among blood donors in Pune, India. J Med Virol. 2019;91(5):813-819.
Crossref - Kenney SP. The Current Host Range of Hepatitis E Viruses. Viruses. 2019;11(5):452.
Crossref - Wang B, Meng XJ. Hepatitis E virus: Host tropism and zoonotic infection. Curr Opin Microbiol. 2020;59:8-15.
Crossref - Gamit M, Patel K, Rathod A, Shrivastav M, Patel B, Vegad M. Hepatitis E virus: Seroprevalence and associated factors in acute viral hepatitis during pregnancy. Int J Med Sci Public Health. 2017;6(3):619-622.
Crossref - Khameneh ZR, Sepehrvand N, Khalkhali H-R. Seroprevalence of Hepatitis E Among Pregnant Women in Urmia, Iran. Hepat Mon. 2013;13(11):e10931.
Crossref - Perez Gracia MT, Suay Garcia B, Mateos Lindemann ML. Hepatitis E and pregnancy: current state. Rev Med Virol. 2017;27(3):e1929.
Crossref - Sivasangeetha K, Geethalakshmi S, Thatchinamoorthy G, Gouthami P, Jacob S. Seroprevalence of Hepatitis E Virus Infection and Their Associated Risk Factors in Pregnant Women in Chennai, Tamil Nadu. Open Forum Infectious Diseases. 2016;3(Suppl 1):423.
Crossref - Renou C, Gobert V, Locher C, et al. Prospective study of Hepatitis E Virus infection among pregnant women in France. Virol J. 2014;11:68.
Crossref - Begum N, Gyaneshwori S, Husain S, Kar P. Seroprevalence of subclinical HEV infection in pregnant women from north India: A hospital based study. Indian J Med Res. 2009;130:709-13.
- Sultana GZ, Moniruzzaman M, Mannan T, Sultana R. Seroprevalence of Subclinical HEV Infection in Healthy Pregnant Urban Dwellers of Bangladesh: Identification of Possible Risk Factors. Journal of Enam Medical College. 2018;8(2):85-89.
Crossref - Singh S, Mohanty A, Joshi YK, Dwivedi SN, Deka D. Outcome of hepatitis E virus infection in Indian pregnant women admitted to a tertiary care hospital. Indian J Med Res. 2001;113:35-39.
- Singh S, Mohanty A, Joshi YK, Deka D, Mohanty S, Panda SK. Mother-to-child transmission of hepatitis E virus infection. Indian J Pediatr. 2003;70(1):37-39.
Crossref - Khaskheli M-N, Baloch S, Sheeba A, Baloch S. Acute Hepatitis E Viral Infection in Pregnancy and Maternal Morbidity. J Coll Physicians Surg Pak. 2015;25(10):734-7.
- Anurada P, et al. Sero Prevalance of hepatitis e virus in patients attending antenatal clinic. Sch J App Med Sci. 2016;4(12B):4311-4317
- Bigna JJ, Modiyinji AF, Nansseu JR, et al. Burden of hepatitis E virus infection in pregnancy and maternofoetal outcomes: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2020;20(1):426.
Crossref - Ma XX, Ji Y, Jin L, et al. Prevalence and clinical features of hepatitis E virus infection in pregnant women: A large cohort study in Inner Mongolia, China. Clin Res Hepatol Gastroenterol. 2021;45(4):101536.
Crossref - Mustafa AAM, Abdalla WM, Ahmed HH, et al. Seroprevalence and Potential Risk Factors of Hepatitis E Virus among Pregnant Women in Khartoum, Sudan. J Pure Appl Microbiol. 2022;16(1):585-592.
Crossref
© The Author(s) 2023. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.