ISSN: 0973-7510
E-ISSN: 2581-690X
Amikacin is an aminoglycoside antibiotic with a broad-spectrum bacterial coverage that is frequently utilized both as monotherapy and in combination with other antibiotics for severe bacterial infections in the paediatric population. The narrow therapeutic index of the drug and high inter-individual variabilities in drug exposure results in either drug toxicity or subtherapeutic concentrations. Thus, therapeutic drug monitoring and population pharmacokinetics are pivotal to facilitate the optimal dosage regimens in paediatrics and negate the adverse outcomes. The therapeutic goal is to maintain the target peak and trough concentrations within 30-40mg/l and <5 mg/l respectively. This review aimed to summarize population pharmacokinetic considerations and the pharmacokinetic parameters of amikacin across the paediatric population.
Amikacin, Paediatric, Population Pharmacokinetics, Therapeutic Drug Monitoring
Aminoglycosides act synergistically against gram-negative organisms and certain gram-positive organisms. These are used for the treatment of severe infections of the abdomen, urinary tract, and respiratory tract infections and can also be used prophylactically.1 Gentamicin and Amikacin are the most frequently used aminoglycosides. Toxicities have been reported due to the increased frequency of Aminoglycoside administration. Several studies have concluded that the once-daily dosing of Aminoglycosides is safe and more efficacious than the multiple dosing.2
Amikacin, a narrow therapeutic index drug, is widely used in the paediatric population for various conditions like neonatal sepsis, hospital-acquired infections, acute respiratory tract infections, and urinary tract infections. It acts by disrupting the protein synthesis and inhibits the growth of bacteria. Due to high inter-individual variability, dosage adjustments are required.3 The most reported toxicities include irreversible ototoxicity and nephrotoxicity which is reversible when detected early. Apart from toxicities, a few adverse effects such as tingling, numbness, fever, rash have been reported.2
Pharmacokinetics is the study of movements of drugs through the body enclosing the kinetics of absorption, distribution, metabolism, and excretion (ADME). The application of pharmacokinetic principles to the safe and effective therapeutic management of the drugs in an individual patient is clinical pharmacokinetics. Primary goals of clinical pharmacokinetics include improving efficacy and reducing the toxicity of patient’s drug therapy. Drug concentration can be measured in the blood or plasma, urine, saliva, and other easily sampled fluids.4-6
Several studies and practice guidelines recommend a target serum Amikacin peak concentration to be 20 to 35 mg/L, trough concentrations >5-10 mg/L.7,14,25 The recommended dosing in neonates and infants is 15mg/kg IV, Once daily (OD) and 7.5mg/kg, twice daily (BD). Comparatively, the OD regimen has reduced toxicity and increased efficacy than the BD regimen.8 Amikacin has a mean half-life of 6.0 hours in neonates and 1.9 hours in children aged up to 6 years.10
Narrow therapeutic drugs tend to cause toxicity. To ensure the safety of the drug a phenomenon called therapeutic drug monitoring (TDM) is performed to optimize the dosage regimen in individual patients.9 To perform TDM, 2 blood samples are collected, one peak sample to be collected 30 mins after drug administration and one trough sample should be collected 1 hour before the next dose, and quantification of the drug is performed.10
High inter-individual variability necessitates the need for Population pharmacokinetic modeling to determine individual Pharmacokinetic parameters and source of variability in a population.11 This review presents the population pharmacokinetics of Amikacin in paediatric population among various age groups and disease conditions.
Literature Search
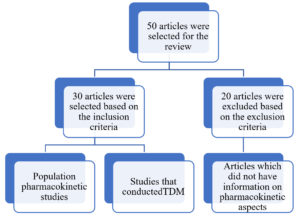
A thorough literature survey was conducted for the time period 1990 to 2021, and 50 articles were identified out of which 30 articles were included and 20 excluded depicted in Figure. The search was conducted in PubMed, Google Scholar, ScienceDirect database engine using the following terms (“aminoglycosides” and “indications”) (“amikacin”), (“amikacin” and “pharmacokinetics”) (“amikacin” and “paediatrics”) (‘amikacin’ and ‘population pharmacokinetics” and “nonlinear mixed effect model”) ( “amikacin” and “neonates”) (“amikacin” and “infants”), (“amikacin” and “disease conditions” and “paediatrics”) (“amikacin” and “dosage optimization”) (“amikacin” and “therapeutic drug monitoring” and “paediatric population”) (“amikacin” and Bayesian modeling”).
Inclusion Criteria
The following studies were included: Studies that conducted therapeutic drug monitoring, Studies that optimized dosage regimens, Studies that determined the population pharmacokinetics in the paediatric population, and Studies that suggested dosage adjustments in different disease conditions.
Exclusion Criteria
The articles which did not have the information on pharmacokinetic aspects were excluded from the study.
Population Pharmacokinetics of Amikacin
High variability in the primary pharmacokinetic parameters influenced by multiple covariates has been established in the paediatric population. Since amikacin excretion is through renal, GFR predominantly determines the clearance values.23 Hence, in neonates there is a significant difference in the clearance of the drug when compared to adults. Gestational age is one such covariate as the preterm infants had higher drug levels than the full-term infants. The mean neonatal amikacin Vd, CL, and t1/2 were 0.78 ± 0.38 l/kg, 86.99 ± 48.22 ml/h·kg, and 6.81 ± 2.51 h, respectively.22 It was evident from a study that there was a decrease in half-life and increase in clearance with increase in the post-conceptional age. Variability has also been noted with the frequency of dosing, for instance, a study conducted by Katarina Vucicevic et al., revealed higher drug levels in the BID dosing viz peak concentration of 36.39 mg/ml and trough concentration of 5.67 mg/ml while the OD regimen produced a peak concentration of 21.79 mg/ml and trough concentration of 3.99 mg/ml respectively.22 The reported mean pharmacokinetic parameters and the influence of covariates among different pop pk studies are summarised in Table 1.
Table (1):
Population Pharmacokinetics among Paediatric Population.
Title |
Covariates |
Equations |
Cpeak(mg/mL) |
Ctrough(mg/mL) |
PK Parameters |
Authors |
|---|---|---|---|---|---|---|
Pharmacokinetic Variability of Amikacin After Once-Daily and Twice-Daily Dosing Regimen in Full-Term Neonates |
Gestational age Body weight Proven sepsis |
C trough= C peak. e–β (𝜏-ti) Cpeak= R0(1-e– β.ti) β.Vd.(1- e–β.𝜏) |
BD GROUP= 21.79 OD GROUP= 36.39 |
BD GROUP=5.67 OD GROUP= 3.99 |
Vd= 0.78 ± 0.38 L/kg Cl= 86.99 ± 48.22 m L/h∙kg T1/2= 6.81 ± 2.51 h |
Katarina Vučićević et al.22 |
Amikacin Pharmacokinetics and Suggested Dosage Modifications for the Preterm Infant |
– |
Tmax. = [ln (Cpeak/Ctrough) I/Kg, (ii) Cave = dose/(Tmax) (CL), (iii) dose = (Cave) (CL). |
C peak= 21.88 ± 4.88 |
C trough= 9.10 ± 3.77 |
Vd=0.57 +0.11l Cl= 0.84 ±0.28 L/kg/hr T1/2= 8.42 ±2.55 h |
Cynthia et al.23 |
Population Pharmacokinetics of Amikacin In Indian Paediatric Patients |
Body weight, age |
CL = 1*(WT/14.2) *EXP ( 1) V = 2*EXP (2) |
– |
– |
Cl=1.23 L/kg/h Vd=3.37 L/kg |
Raju et al.24 |
*Ctrough -Trough Concentration, Cpeak – Peak Concentration, Tmax – Time taken to reach the maximum concentration, Cave– Average Concentration, Vd – Volume of Distribution, Cl – Clearance
Dosage Adjustments and Pharmacokinetics of Amikacin in Various Disease Conditions
Amikacin has been used in various disease conditions and it is often co-administered with other antibiotics including Vancomycin, beta-lactam antibiotics. There is a higher inter-individual variability observed in ALL when compared to the normal healthy volunteers.12 The mean peak serum concentrations were observed to be 36.30±4.03 µg/ml. normal healthy volunteer- 19 to 43.8 mg/L. due to morphological changes in cancer patients, the renal clearance might be affected which has a direct effect on the clearance of the drug. The clearance and half-life tend to decrease in oncology patients which stated the importance of optimizing the dose of amikacin in paediatric all patients.
In paediatric population, amikacin is widely used to treat sepsis and the patients at risk of sepsis. The burn patients’ pathogenesis might result in altered vd, cl of amikacin.13 A total of 73 burn patients were included in a study to determine the pharmacokinetics of amikacin in burn patients. the multivariate analysis revealed that bodyweight-only had a significant effect on clearance and other covariates like age, sex, concomitant adm with vancomycin had no effect on cl or Vd. Also, pharmacodynamic studies should be conducted in burn patients to optimize the dosage. Drug characteristics such as weight, lipophilicity, and pH have an impact on the disease condition. In preterm and term neonates, at birth, the volume of distribution is increased but did not influence clearance. An increase in peak concentrations and lower trough concentrations suggested dosage adjustment in pre-term and term neonates.14
In Perinatal Asphyxia Treated with Hypothermia, there is a substantial decrease in the clearance of the drug by 40.6% but no change was noted in the volume of distribution. The percentage of neonates with toxic trough levels had decreased from 40 to 76% to 14 to 25% by increasing the dosing interval by 12h. Simulation of the study revealed that the neonates reaching the toxic trough levels has decreased by increasing the dosing interval by 12h which also increased the clearance. For children weighing 2.8kg, the dose recommended was 15mg/kg every 42h and 15mg/kg every 48hours for children weighing between 1.8kg to 2.8kg.15 Parameters of the above-discussed disease condition have been shown in the Table 2.
Table (2):
Pharmacokinetic Parameters in Various Disease Conditions.
| Disease condition | Age | Bodyweight | Peak conc. | Trough conc. mg/mL | AUC (µg.hr/ml) | Clearance | Volume of Distribution | Half life (h) | Authors |
|---|---|---|---|---|---|---|---|---|---|
| Febrile Neutropenia | 3-11 | 11.5-21.5 | 36.30 ± 4.03 | 0.41 ± 0.23 | 76.20±6.30 | 18.85±5.11 mL/min | 0.19±0.11 L/kg | 1.76±0.55 | Nadeem et al.12 |
| Burn Patients | 0.6–17 | 8-90 | 33.2 ± 9.4 | 3.8± 4.6 | – | 2.48 L/h | 2.71 L | – | Catherine et al.13 |
| Sepsis | 0.16–21.75 (h) | (0.9–5.2 | 17.5 ± 9.3T | 6.2± 3.4 | – | 0.153L/h | 2.94L | 13.7 | Amponsah et al.14 |
| 19.9 (10.5) P | 9.2 ± 5.7 | ||||||||
| Perinatal asphyxia treated with hypothermia | 0.22 (8) | 0.926 (2) | – | – | – | 0.0495 (2) | 0.832(1) | – | Sinziana et al.15 |
*AUC- Area under the curve
Therapeutic Drug Monitoring of Amikacin to Assess Nephrotoxicity & Ototoxicity
Commonly reported toxicities of Amikacin are nephrotoxicity and ototoxicity. Several studies have been conducted to compare the safety and efficacy of once-daily and twice-daily dosing of Amikacin.16 It has been established that the trough plasma concentration of <10mg/L is safer and there exists a risk of ototoxicity when it exceeds 10mg/L and duration of therapy if it exceeds more than 7 days. The peak plasma concentration of up to 30mg/L is acceptable. Amikacin-induced ototoxicity is caused by damaging the cochlea in the inner ear which is known as cochleotoxicity leading to permanent hearing loss. It also causes calcium influx by binding to the NMDA receptors. Tinnitus is used in the early diagnosis of ototoxicity in paediatric patients.17 Extremely low-birth-weight infants are at higher risk for ototoxicity compared to low birth-weight infants. Thus, dosage adjustments of Amikacin are needed based on the gestational age, birth weight.18
Nephrotoxicity is yet another familiar toxicity of Amikacin predisposed by the accumulation of the drug in the proximal renal tubule, which produces oxidative damage by emitting free radicals.19 The risk of toxicity is typically more with the coadministration of other nephrotoxic drugs such as loop diuretics, NSAIDs, Amphotericin B, etc. nephrotoxicity was assessed by serum creatinine levels if >0.3mg/dl or 50% increase after the initial therapy. The simulation studies revealed significantly high variability between the plasma levels in preterm and term infants. Thus, higher risk in preterm infants than the term infants those with increased serum Amikacin levels in preterm infants have been concluded.20
Monitoring of Ototoxicity and Nephrotoxicity
Ototoxicity is measured by an otoacoustic emission test and pure tone screening. It is screened by using audiometry, earphones. It is managed by audiological interventions such as hearing aids, educational interventions, and tinnitus therapy.18 For the prevention of nephrotoxicity, calculating creatinine clearance, baseline kidney function, and urinary alpha-1m excretion should be monitored in all the patients administered with Amikacin and therapeutic drug monitoring is essential in patients with abnormal renal function.21
Once Daily (OD) vs Twice Daily (BD) Dosing of Amikacin
There has been a conflicting view about the safety of once-daily vs twice-daily regimens. Studies have stated that mean peak and trough concentrations 21.79 μg/ml and 5.67 μg/ml in twice-daily regimen was significantly different from peak and trough concentrations of 36.39 μg/ml and 3.99 μg/ml of once-daily regimen but there was no change observed in the pharmacokinetic parameters.22 Some studies have concluded that the OD regimen had higher peak concentrations and less trough concentration compared to the twice-daily regimen.16 When the peak plasma concentration is higher the activity of the drug will be higher, at the same time when the trough level is below 10 mg/L ototoxicity can be prevented.23 Thus, establishing the superiority of the once-daily regimen owing to higher bactericidal effect with higher peak plasma concentration and better tolerability with lower trough plasma concentrations.
Amikacin is a narrow therapeutic drug with high inter-individual variability. Pharmacokinetic modeling enables the individualization ratio of dosage regimens. High variability has been observed in the clearance and volume of distribution in preterm and term infants. Thus, this review article concludes that Amikacin should be administered only when it is indicated, and dosing should be rational as the Amikacin pharmacokinetic parameters. Therapeutic drug monitoring of Amikacin is necessary to optimize a safe and effective dose. Thus, further studies have to be conducted to recommend an appropriate dose for safe and effective treatment of Amikacin in paediatric population.
ACKNOWLEDGMENTS
The authors would like to thank Department of Pharmacy Practice, JSS College of Pharmacy, Ooty for their extended support and cooperation.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
KC and KPA have formulated the hypothesis. TN, HV and SNK collected the articles and wrote the manuscript. All authors read and approved the final manuscript for publication.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript.
ETHICS STATEMENT
Not applicable.
- Becker B, Cooper MA. Aminoglycoside antibiotics in the 21st century. ACS Chem Biol. 2013;8(1):105-115.
Crossref - Gonzalez LS, Spencer JP. Aminoglycosides: a practical review. Am Fam Physician. 1998;58(8):1811-1820.
- Sizar O, Rahman S, Sundareshan V. Amikacin. StatPearls. 2021. Accessed 15 November 2021. http://www.ncbi.nlm.nih.gov/books/NBK430908/
- Clinical Pharmacokinetics and Pharmacodynamics Pharmacotherapy: A Pathophysiologic Approach, 10e. Access Pharmacy, McGraw Hill Medical. https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=146077432. Accessed 15 November 2021.
- Pharmacokinetics – an overview | ScienceDirect Topics. https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/pharmacokinetics. Accessed 15 November 2021.
- Venkateswarlu V, Biopharmaceutics and Pharmacokinetics, 2nd ed. Hyderabad, India. Pharma Med Press. 2018.
- du Toit M, Burger JR, Rakumakoe DM, Rheeders M. Standards of aminoglycoside therapeutic drug monitoring in a South African private hospital: perspectives and implications. Ghana Med J. 2019;53(1):8-12.
Crossref - Hughes KM, Johnson PN, Anderson MP, Sekar KC, Welliver RC, Miller JL. Comparison of Amikacin Pharmacokinetics in Neonates Following Implementation of a New Dosage Protocol. J Pediatr Pharmacol Ther. 2017;22(1):33-40.
Crossref - Pacifici GM, Marchini G. Clinical Pharmacology of amikacin in infants and children. Clin Med Invest. 2019;5(1).
Crossref - Mould DR, Upton RN. Basic Concepts in Population Modeling, Simulation, and Model-Based Drug Development – Part 2: Introduction to Pharmacokinetic Modeling Methods. CPT Pharmacometrics Syst Pharmacol. 2013;2(4):1-14.
Crossref - Bukhari NI, Yousuf SA, Jamshaid MU, MUSTAFA M. Pharmacokinetics of amikacin in febrile neutropenic pediatric patients with acute lymphoblastic leukaemia. Turkish J Cancer. 2001;31:114-120.
- Illamola SM, Sherwin C, Van Hasselt C. Clinical Pharmacokinetics of Amikacin in Pediatric Patients: A Comprehensive Review of Population Pharmacokinetic Analyses. Clinical Pharmacokinetics. 2018;57:1-12.
Crossref - Amponsah SK, Adjei GO, Enweronu-Laryea C, et al. Population Pharmacokinetic Characteristics of Amikacin in Suspected Cases of Neonatal Sepsis in a Low-Resource African Setting: A Prospective Nonrandomized Single-Site Study. Curr Ther Res Clin Exp. 2017;84:e1-e6.
Crossref - Cristea S, Smits A, Kulo A, et al. Amikacin Pharmacokinetics To Optimize Dosing in Neonates with Perinatal Asphyxia Treated with Hypothermia. Antimicrob Agents Chemother. 2017;61(12):e01282-17.
Crossref - Abdel-Hady E, El Hamamsy M, Hedaya M, Awad H. The efficacy and toxicity of two dosing-regimens of amikacin in neonates with sepsis. J Clin Pharm Ther. 2011;36(1):45-52.
Crossref - Chen KS, Bach A, Shoup A, Winick NJ. Hearing loss and vestibular dysfunction among children with cancer after receiving aminoglycosides. Pediatr Blood Cancer. 2013;60(11):1772-1777.
Crossref - Endo A, Nemoto A, Hanawa K, et al. Relationship between amikacin blood concentration and ototoxicity in low birth weight infants. J Infect Chemother. 2019;25(1):17-21.
Crossref - Kim DJ, Lee J, Yu H, et al. Nephrotoxicity of amikacin in noncritically ill patients. Clin Nephrol. 2019;92(4):201-207.
Crossref - Kaynar K, Gul S, Ersoz S, Ozdemir F, Ulusoy H, Ulusoy S. Amikacin-induced nephropathy: is there any protective way? Ren Fail. 2007;29(1):23-27.
Crossref - Siddiqi A, Khan DA, Khan FA, Razzaq A. Therapeutic drug monitoring of amikacin in preterm and term infants. Singapore Med J. 2009;50(5):486-489.
- Vucicevic K, Rakonjac Z, Miljkovic B, Jankovic B, Prostran M. Pharmacokinetic Variability of Amikacin After Once-Daily and Twice-Daily Dosing Regimen in Full-Term Neonates. J Pharmacol Sci. 2014;124(2):138-143.
Crossref - Kenyon CF, Knoppert DC, Lee SK, Vandenberghe HM, Chance GW. Amikacin pharmacokinetics and suggested dosage modifications for the preterm infant. Antimicrob Agents Chemother. 1990;34(2):265-268.
Crossref - Akondi RB, Chodavarapu RK, Devarakonda KR. Population Pharmacokinetics of Amikacin in Indian Pediatric Patients. Clinical Research and Regulatory Affairs. 2008;25(3):173-182.
Crossref - Smits A, Kulo A, van den Anker J, Allegaert K. The amikacin research program: a stepwise approach to validate dosing regimens in neonates. Expert Opin Drug Metab Toxicol. 2017;13(2):157-166.
Crossref
© The Author(s) 2022. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.