ISSN: 0973-7510
E-ISSN: 2581-690X
Given the magnitude of the COVID-19 pandemic, adverse psychological outcomes are expected to occur among healthcare personnel (HCPs). However, little is known about these outcomes within Ras al Khaimah, UAE. This study aims to assess the psychological impact of COVID-19 on healthcare personnel from different hospitals and clinics in Ras Al Khaimah (RAK), UAE. An online questionnaire was distributed to healthcare personnel within Ras al Khaimah, UAE, through an institutional email that enabled them to enroll in the study after giving informed consent. Likert scale was used to calculate the relation between demographic factors and 13 variables of psychological distress. An unpaired t-test was applied. This study shows that 31.7% of HCPs in RAK report moderate to high levels of anxiety due to concerns of potential workplace exposure, 41.6% are afraid of infecting their families and 13.1% find themselves feeling isolated from their families. Those who were younger than 45 years old, unmarried people and having more than two children were more likely to experience psychological distress than their counterparts. While the adverse psychological impact within this population is not as severe as what was noted in different populations in other countries, they must be addressed. It is important to ensure that HCPs have the appropriate physical and mental resources to persevere through similar stressful periods in the future.
Psychological Distress, Healthcare Workers, Healthcare Personnel, Ras al Khaimah, UAE, Questionnaire
The COVID-19 pandemic has wreaked havoc on the healthcare industry causing deaths of millions of people around the world. As of August 2023, over 769 million laboratory-tested COVID-19 cases and 6.9 million deaths have been reported globally. As of December 2023, 1.6 million cases were diagnosed and 2,349 deaths were recorded in the United Arab Emirates.1-3
Previous studies have linked the outbreaks of infectious diseases, such as COVID-19, MERS, Ebola, H7N9, H1N1 and SARS with post-traumatic stress symptoms (PTSS) and other adverse psychological symptoms. Mandatory or self-imposed quarantine, social isolation, fear of infection, lack of supplies and financial loss increase the risk of mental disorders such as depression, anxiety, thought disorders and post-traumatic stress, and healthcare workers are not immune to this stress. Inadequate personal protective equipment (PPEs), staff shortages, and frequent exposure to patients’ suffering and dying are some of the other challenges frequently encountered by healthcare workers. Lack of emotional support and negative coping strategies lead to the exacerbation of mental health problems.4-6
In China, 77.3% of frontline nurses had suffered anxiety symptoms, with the severity of anxiety depending on length of service and clinical working time. Meanwhile, in the United States of America, 63.38% of healthcare workers reported mild to clinically meaningful anxiety, 46.61% reported mild to severe depressive symptoms, 5% endured suicidal ideation and 14% screened positive for post-traumatic stress disorder (PTSD).7,8
Within the United Arab Emirates, a study in Sharjah reported that during the COVID-19 pandemic, frontline workers were more likely to suffer high levels of anxiety. Another study found that a larger percentage of HCPs in UAE suffered depression due to COVID-19 in comparison to the other Arab countries.9,10
However, little is known about the psychological impact of the COVID-19 pandemic on medical workers in other parts of the UAE. It is necessary to gather data on this matter to help facilitate programs and provide resources to alleviate stress and ensure their psychological well-being in the event of future medical emergencies. It will also provide prospective physicians and nurses an understanding on what to expect as professionals in times of such emergencies in the future.
Objective
To assess the psychological impact of COVID-19 on healthcare personnel from different hospitals and clinics in Ras Al Khaimah, UAE.
It was a cross-sectional study performed in various hospitals all over UAE conducted during November 2020 to February 2021. The study subjects were Frontline health care personnel from various medical institutions, clinics and hospitals across Ras Al Khaimah. Data could be collected from 82 participants which included people from different professions like doctors, nurses, teaching faculty, technicians and other staff members such as occupational therapists, administrative staff and maintenance staff. The study did not exclude potential subjects from participation on the basis of ethnic origin or gender. Subjects included men, women, and all ethnic origins, provided they met all eligibility criteria as follows:
- They practiced as health care medical professionals.
- They were dealing with COVID-19 patients/potential COVID-19 patients.
- They lived/practiced in Ras al Khaimah.
Convenience sampling was used to select the study participants.
An online questionnaire was constructed by the student investigators and distributed among faculty staff for their advice. The questionnaire was revised based on their feedback and was recirculated among 15 faculties for their final review. This final version of the questionnaire was then distributed through an institutional email that enabled the target population to enroll in the study after giving informed consent. An online consent form was displayed at the beginning of the online questionnaire; if participants had no objection to the objectives of the survey, they would officially start the survey by clicking the “Start” button below, or they had the right to withdraw from the survey. Each participant was only allowed to answer the questionnaire once.
The questionnaire collected the following details:
Socio-demographic details included the following
Gender, Age, Occupation, Current living situation.
COVID-19 emergency-related psychological factors
Single items measured through pointed scale from 1-5. COVID-19 emergency-related psychological factors included fear of COVID-19 infection due to work-related exposure.
Psychological distress
The various psychological effects of COVID-19 were estimated on a 5-point scale. Part I of the questionnaire has a scale ranging from 1 to 5 (1-Not at all, 2-Slightly, 3-Neutral, 4-Extremely, 5-Extremely) which measures the intensity of the psychological impacts of COVID-19 on the healthcare workers whereas Part II has a scale (1-Never, 2-Rarely, 3-Sometimes, 4-Mostly, 5-Always) measuring the frequency of the effects. Higher values indicate higher psychological distress.
Analysis of main outcome and process measures compared front line healthcare workers in different work spaces all over RAK depending on the profession, severity of the daily challenges etc. Graphical representation was produced depending on the conclusion of the study.
Likert scale was used to calculate the relation between different demographic factors and 13 variables of psychological distress. The mean value of all the questions was measured and standard deviation calculated; following which an unpaired t-test was applied.
Survey details
Socio-demographic details:
i). Age
ii). Gender
iii). Place of work
iv). Marital status
v). Profession
vi). Number of children
vii). Current living situation
viii). History of COVID-19 infection
ix). Family history of COVID-19 infection
x). Change in living situation during the COVID-19 pandemic
xi). Use of antidepressant medications
COVID-19 pandemic related social factors: 5-point scale (1-Not at all, 2-Slightly, 3-Neutral, 4-Extremely, 5-Extremely) where the higher value indicates higher effect.
i). Effect of COVID-19 pandemic on personal relationships
ii). Effect of negligence of public regarding COVID-19 regulations
iii). Change in perception of profession due to COVID-19 pandemic
iv). Change in family’s perception of profession due to COVID-19 pandemic
v). Change in viewpoint of COVID-19 infection from initial outbreak
(vi). Change in personal hygiene practices due to COVID-19 pandemic
COVID-19 pandemic related psychological factors: 5-point scale (1-Never, 2-Rarely, 3-Sometimes, 4-Mostly, 5-Always) where the higher value indicates higher effect.
i). Feeling deprived of attention of personal relations
ii). Personal relations feeling deprived of respondent’s attention
iii). Feelings of anxiety due to potential workplace exposure to COVID-19 virus
iv). Feelings of anxiety due to potentially spreading COVID-19 virus to personal relations
v). Difficulty relaxing due to COVID-19 pandemic
vi). Experiencing acute increase in stress due to COVID-19 pandemic
vii). Feelings of hopelessness related to COVID-19 pandemic.
Limitations/expected challenges
1. Respondents found it difficult to complete the questionnaire due to busy working schedules.
2. Gathering data and finding respondents who would volunteer to participate in this study.
Of the 82 responses received, 60 were accepted in accordance with the eligibility criteria described in the Methods-Selection criteria. Table 1 shows their demographic characteristics.
Table (1):
Distribution of respondents according to Socio-demographic profile
| Demographic Profile | No. n=60 | % |
|---|---|---|
| Age Group | ||
| 25-30 | 12 | 20.0 |
| 31-35 | 8 | 13.3 |
| 36-40 | 6 | 10.0 |
| 41-45 | 11 | 18.3 |
| 46-50 | 7 | 11.7 |
| 51-55 | 8 | 13.3 |
| 56-60 | 2 | 3.3 |
| 61-65 | 3 | 5.0 |
| 65+ | 3 | 5.0 |
| Gender | ||
| Male | 25 | 41.7 |
| Female | 35 | 58.3 |
| Profession | ||
| Doctor | 33 | 55.0 |
| Nurse | 9 | 15.0 |
| Nursing Faculty | 5 | 8.3 |
| Pharmacy Faculty | 3 | 5.0 |
| Technical Staff | 5 | 8.3 |
| Other Staff | 5 | 8.3 |
| Marital Status | ||
| Married | 46 | 76.7 |
| Single | 14 | 23.3 |
| No. of Children | ||
| One | 9 | 15.0 |
| Two | 23 | 38.3 |
| Three | 7 | 11.7 |
| More than Three | 4 | 6.7 |
| None | 17 | 28.3 |
*The largest demographic in each circumstance has been underlined.
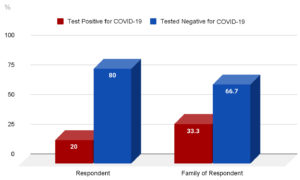
Figure 1 shows the percentage of the respondents and their family members who were infected with the COVID-19 virus. Of the respondents who tested positive, 25% of them experienced PTSD symptoms.
20% of the respondent’s tested positive for COVID-19 infection and 33.3% of respondents’ families tested positive for the COVID-19 infection.
Table (2):
Distribution of respondents according to living situation before and during the pandemic
| Living situation before pandemic | Living situation during pandemic | |||
|---|---|---|---|---|
| No. (n=60) | Percentage | No. (n=60) | Percentage | |
| Alone | 10 | 16.7 | 14 | 23.3 |
| Extended family | 6 | 10.0 | 4 | 6.7 |
| Friends/colleagues | 2 | 3.3 | 2 | 3.3 |
| Parents | 6 | 10.0 | 4 | 6.7 |
| Spouse | 6 | 10.0 | 7 | 11.7 |
| Spouse & child/children | 30 | 50.0 | 29 | 48.3 |
*Most respondents lived with their spouse and child/children before and during the pandemic.
5 respondents elected to move out from a shared living situation to single accommodation, 2 respondents left their extended family and moved in with their spouse, 1 respondent left their single accommodation and moved in with their spouse and child/children.
Table 2 describes the living situations of respondent’s before and during the pandemic. Before the pandemic, 16.7% of the HCPs lived alone and 83.3% of the HCPs lived in a group/family setting. During the pandemic the number of HCPs residing with others decreased by 6.6%. 4(8.2%) of the 60 respondents were on antidepressants.
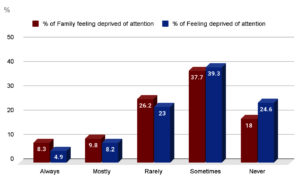
Figure 2. Distribution of respondents according to feeling of attention deprivation by and from family
*Most respondents claim that their family sometimes feels deprived of their attention.
Most respondents also report sometimes feeling deprived of their family’s attention.
Figure 2 shows the distribution of respondents and their families feeling deprived of attention.
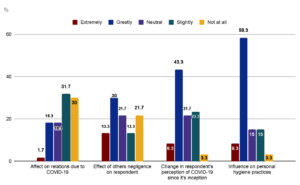
Figure 3. Distribution of respondents according to social factors
*Most respondents say that they have noticed a slight change in their relationships due to the COVID-19 and a great effect of other’s negligence in regards to COVID-19 safety regulations.
They note that their perception of COVID-19 has greatly changed since the start of the pandemic and that they have made great changes in personal hygiene practices due to it.
Figure 3 describes the responses of 4 factors – Effect on relationships due to the pandemic, effect of the public’s negligence in regards to the COVID-19 prevention measure, change in perception of the COVID-19 infection since its inception and influence of the pandemic on personal hygiene.
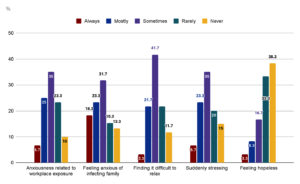
Figure 4. Distribution of respondents according to 5 factors (Anxiousness, difficulty relaxing, sudden stress, hopelessness)
*Most respondents claim to sometimes feel anxiety due to workplace exposure to COVID-19 virus or due to fear of them infecting their families with COVID-19 virus. They also sometimes find it difficult to relax due to the COVID-19 pandemic and find themselves having moments of sudden stress due to the COVID-19 pandemic. However, they report never feeling hopeless in the face of the COVID-19 pandemic.
Figure 4 depicts the responses according to 5 factors – anxiousness due to fears of workplace exposure or of infecting family, difficulty in relaxing, moments of sudden stress and feelings of hopelessness in the face of the pandemic.
Likert scale was used to calculate the relation between the above-mentioned demographic factors and the 13 variables of psychological distress. The mean value of all the questions was measured and standard deviation was calculated; following which an unpaired t-test was applied. The values are provided in Table 3.
Table (3):
Findings of the Likert scale and unpaired t-test
| Association of elements of psychological stress with demographic factors | Profession | Age | Marital status | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. | Mean±SD | P value | No. | Mean±SD | P value | No. | Mean±SD | P value | |
| Effect on personal relationships due to the COVID-19 pandemic | Dr. (33) | 2.33 ±1.18 | 1 | ≤ 45 (37) | 2.54 ±1.14 |
0.04 | Single (14) | 2.92 ±1.14 |
0.02 |
| Non- Dr. (27) | 2.33 ±1.18 | > 45 (23) | 1.9 1±1.14 |
Married (46)  | 2.1 ±1.14 |
||||
| Feeling deprived of attention from close relations due to protection measures taken during the COVID-19 pandemic | Dr. (33) | 2.48 ±1.11 | 0.78 | ≤ 45 (37) | 2.70 ±1.11 |
0.02 | Single (14) | 2.92 ±1.11 | 0.6 |
| Non- Dr. (27) | 2.4 ±1.11 | > 45 (23) | 2.04 ±1.11 |
Married (46) | 2.3 ±1.11 | ||||
| Awareness of close relations feeling deprived of attention due to protection measures undertaken during the COVID-19 pandemic | Dr. (33) | 2.63 ±1.13 | 0.89 | ≤ 45 (37) | 2.91 ±1.14 |
0.01 | Single (14) | 3.28 ±1.14 |
0.02 |
| Non- Dr. (27) | 2.59 ±1.13 | > 45 (23) | 2.13 ±1.14 |
Married (46) | 2.41 ±1.14 |
||||
| Effect of the negligence of others in protection measures on respondent | Dr. (33) | 2.93 ±1.34 | 0.77 | ≤ 45 (37) | 3.29 ±1.37 |
0.01 | Single (14) | 4± 1.37 |
0.004 |
| Non- Dr. (27) | 3.03 ±1.34 | > 45 (23) | 2.52 ±1.37 |
Married (46) | 2.69 ±1.37 |
||||
| Anxiousness due to work-place exposure to the COVID-19 virus | Dr. (33) | 2.93 ±1.08 | 0.91 | ≤ 45 (37) | 3.27 ±1.08 |
0.005 | Single (14) | 3.5 ±1.08 |
0.03 |
| Non- Dr. (27) | 2.96 ±1.08 | > 45 (23) | 2.43 ±1.08 |
Married (46) | 2.78
±1.08 |
||||
| Anxiousness of potentially infecting family/friends with the COVID-19 virus | Dr. (33) | 3.24 ±1.27 | 0.76 | ≤ 45 (37) | 3.56 ±1.27 |
0.006 | Single (14) | 3.71 ±1.27 | 0.08 |
| Non- Dr. (27) | 3.14 ±1.27 | > 45 (23) | 2.60 ±1.27 |
Married (46) | 3.04 ±1.27 | ||||
| Difficulty relaxing due to the COVID-19 pandemic | Dr. (33) | 2.72 ±1.01 | 0.38 | ≤ 45 (37) | 3.05 ±1.01 |
0.03 | Single (14) | 3 ±1.01 | 0.43 |
| Non- Dr. (27) | 2.95 ±1.01 | > 45 (23) | 2.47 ±1.01 |
Married (46) | 2.76 ±1.01 | ||||
| Experiencing moments of sudden stress related to the COVID-19 pandemic | Dr. (33) | 2.84 ±1.14 | 0.68 | ≤ 45 (37) | 3.18 ±1.41 |
0.03 | Single (14) | 3.42 ±1.15 | 0.06 |
| Non- Dr. (27) | 2.96 ±1.14 | > 45 (23) | 2.34 ±1.41 |
Married (46) | 2.74 ±1.15 | ||||
| Feelings of hopelessness related to the COVID-19 pandemic | Dr. (33) | 2.06 ±1.07 | 0.82 | ≤ 45 (37) | 2.29 ±1.09 |
0.03 | Single (14) | 2.64 ±1.09 |
0.02 |
| Non- Dr. (27) | 2 ±1.07 | > 45 (23) | 1.65 ±1.09 |
Married (46) | 1.86 ±1.09 |
||||
| Change in viewpoint of the COVID-19 pandemic since it’s start | Dr. (33) | 3.18 ±1.03 | 0.33 | ≤ 45 (37) | 3.54 ±1.03 |
0.02 | Single (14) | 3.71 ±1.03 | 0.09 |
| Non- Dr. (27) | 3.44 ±1.03 | > 45 (23) | 2.91 ±1.03 |
Married (46) | 3.17 ±1.03 | ||||
| Respondent’s change in perception of profession | Dr. (33) | 3.06 ±1.18 | 0.92 | ≤ 45 (37) | 3.32 ±1.18 | 0.02 | Single (14) | 3.71 ±1.19 |
0.02 |
| Non- Dr. (27) | 3.03 ±1.18 | > 45 (23) | 2.60 ±1.18 | Married (46) | 2.86 ±1.19 |
||||
| Respondent’s close relations changes in perception of profession | Dr. (33) | 3 ±1.94 | 0.6 | ≤ 45 (37) | 3.13 ±1.2 | 0.05 | Single (14) | 3.14 ±1.19 | 0.35 |
| Non- Dr. (27) | 2.74 ±1.94 | > 45 (23) | 2.5 ±1.2 | Married (46) | 2.8 ±1.19 | ||||
* The relevant findings have been underlined.
Profession
Our results do not show any relation between profession and psychological distress.
Age
The results showed that HCPs younger than 45 years were more likely to have psychological distress. Their responses showed that the pandemic had affected their personal relationships, causing them to feel deprived of attention from their family and friends. They also noticed that their family members and friends were feeling deprived of attention as well; which could be related to the respondent maintaining their distance from their close ones in an attempt to prevent them from being infected with the COVID-19 virus. Younger people also tend to be more anxious about work-place exposure to the COVID-19 virus; and also, about potentially infecting their close ones. They also feel a lot more frustrated about the negligence of others in maintaining appropriate COVID-19 safety measures. This could be attributed to exposure levels. Older healthcare professionals were less likely to be on the front-lines, reducing their exposure and hence their stress levels. The same cannot be said for the younger professionals. Another factor could be experience. Those who were younger likely felt more fear due to how unpredictable the pandemic was, whereas those older might have felt more comfortable by relying on their medical expertise, particularly prior experiences with epidemics like HIV/AIDS and the H2N2 pandemics, to guide them through those unpredictable factors. If more personal factors were to be taken into consideration, the younger respondents perhaps were more shaken at the deaths caused by the pandemic, whereas the older respondents have had a longer career and hence more time to learn how to process the death of a patient and the turmoil that causes.5,11-14
Marital status
Single people tend to have more psychological distress than those who are married. They noted a change in their personal relationships due to the pandemic. They are also aware that their friends and family members feel deprived of their attention, largely due to protective measures that the respondents had undertaken to prevent spreading the infection. Single people also noted a greater tendency to feel anxious due to the threat of work-place exposure to the COVID-19 virus. They feel frustrated when others do not maintain appropriate protective and social distancing measures, potentially spreading the virus. They feel hopeless in the face of the pandemic, expressing that they feel differently about their profession when compared to before the pandemic began.
The reasons for this increased stress could be attributed to a lack of company. The pandemic caused people, particularly healthcare workers, to socially and physically distance themselves from friends and family in order to limit the spread of the virus, resulting in isolation. This isolation could be reduced if the respondent was living with their spouse and/or children. They could also more easily distract themselves and not focus too deeply at the pandemic at home, a contrast to those who were not married.15,16
Number of children
Out of all the respondents who had children, those with more than 2 children felt particularly lonely and were aware of their close ones feeling neglected by the respondent. They also noticed that their friends/family members began viewing them differently due to factors related to the pandemic. They were more likely to feel anxious about potentially infecting their families and were more upset when others displayed negligence regarding precautions aimed at reducing the spread of the COVID-19 virus. They have had a significant change in viewpoint with regards to the pandemic and are more likely to feel hopeless in its face. There could be multiple reasons for these findings. For one, schools and universities shifted to online learning during the pandemic. Accommodating to the academic needs of each child could be stressful within a single house. The children would also undoubtedly be restless cooped up inside their homes, creating tensions within the house. The lack of a caretaker or nanny could also mean that the children demanded all spare attention, reducing the time the respondent had to themselves. There is also the risk of spreading infections. A young child is not likely to isolate themselves from their family members if they were infected with the virus. A few healthcare personnel also suffered from pay-cuts during the pandemic, due to the economic crisis that resulted. This could mean that the respondent was more stressed about the future of their children.6
A study in Sharjah found that 37% of healthcare workers reported moderate to severe psychological distress. Their main triggers for anxiety were concerns about spreading COVID-19 infection to their family, fears of getting infected with the virus and being isolated.9 HCPs in RAK reported similar concerns, with 31.7% reporting moderate to high levels of anxiety due to concerns of potential workplace exposure, 41.6% afraid of infecting their families and 13.1% feeling isolated from their families. In contrast, in the UK, 67% of the participants felt that being in the workplace increased their risk of catching the virus, despite the numerous safety measures. 88% of HCPs in the UK were concerned about being infected with the virus, while 78% of them were worried about passing the virus to their close ones.6 Meanwhile, 2.17% of Chinese HCPs reported an increased incidence in severe anxiety, 4.78% reported moderate anxiety and mild anxiety was reported by 16.09%. This study also found that the incidence of stress disorder in medical staff was 27.39%.15
In a study conducted in Italy, a total of 21.90% reported high perceived stress and 19.80% reported symptoms of anxiety. Said study even noted that being exposed to contagion was associated with symptoms of depression, a finding echoed in a different study in Maryland, USA; which noted higher post-traumatic stress symptoms in HCPs who were in direct contact with COVID-19 patients.17,18
In a national study conducted in the United States of America, 33% reported clinically meaningful anxiety. The same study found that 17% of their respondents expressed moderate to severe depressive symptoms. Most disturbingly, 4% of the participants reported suicidal ideation.18
Younger respondents in the UK, Italy and in our study noted that the pandemic had affected their mental health. They were more likely to feel anxious and heavily stressed.6,19
These results show that those who were younger than 45 years old were more likely to experience psychological distress than those older, which could be a consequence of differing exposure levels to the COVID-19 virus, and a significant difference in intellectual and emotional experiences.
It also shows that unmarried people tend to have more psychological distress than those who were married, likely due to the company and support of a loved one.
Finally, these results suggest that respondents with more than two children are more at risk for psychological distress. This could be attributed to the difficulty in accommodating the academic and emotional needs of each child, reducing personal time. It could also be due to straining financial situations as a consequence of the pay-cuts and lay-offs that the economic crisis caused.
ACKNOWLEDGMENTS
The authors would like to thank Data & Statistics Department, Emirates Health Services – UAE for their support.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript.
ETHICS STATEMENT
This study is reviewed and approved by the Data & Statistics Department, Emirates Health Services – UAE and the Institutional Ethics Committee, RAKMHSU-REC and RAK-REC (MOHAP/REC/2020/70-2020-UG-M).
INFORMED CONSENT
Written informed consent was obtained from the participants before enrolling in the study.
- www.who.int. Weekly epidemiological update on COVID-19. 2023. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19 Accessed 10 August 2023
- Sekar P, Menezes GA, Shivappa P, George BT, Hossain A. Considerations in Real-time Reverse Transcription Polymerase Chain Reaction (rRT-PCR) for the Detection of SARS-CoV-2 from Nasopharyngeal Swabs. J Pharm Res Int. 2021;33(17):68-78.
Crossref - Ncema.gov.ae. UAE Coronavirus (COVID-19) Updates; 2020. [online] Available at: https://covid19.ncema.gov.ae/en.
- Qiu D, Li Y, Li L, He J, Ouyang F, Xiao S. Infectious Disease Outbreak and Post-Traumatic Stress Symptoms: A Systematic Review and Meta-Analysis. Front Psychol. 2021;12:668784.
Crossref - Samartha K, Rebecca K, Louise E. The psychological impact of quarantine and how to reduce it: rapid review of evidence. Lancet. 2020;395:912-920.
Crossref - Eddy CM. The social impact of COVID-19 as perceived by the employees of a UK mental health service. Int J Ment Health Nurs. 2021;30(S1):1366-1375.
Crossref - Li R, Chen Y, Lv J, et al. Anxiety and related factors in frontline clinical nurses fighting COVID-19 in Wuhan. Medicine. 2020;99(30):e21413.
Crossref - Young KP, Kolcz DL, O’Sullivan D, Ferrand J, Fried JS, Robinson KJ. Health Care Workers’ Mental Health and Quality of Life During COVID-19: Results From a Mid-Pandemic, National Survey. Psychiatr Ser. 2021;72(2):122-128.
Crossref - Saddik B, Elbarazi I, Temsah MH, et al. Psychological Distress and Anxiety Levels Among Health Care Workers at the Height of the COVID-19 Pandemic in the United Arab Emirates. Int J Public Health. 2021;66:1604369.
Crossref - Titi MA, Wahabi H, Elmorshedy H, et al. Mental health impact of the first wave of COVID-19 pandemic on healthcare workers in 12 Arab countries. East Mediterr Health J. 2022;28(10):707-718.
Crossref - Tam CWC, Pang EPF, Lam LCW, Chiu HFK. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. 2004;34(7):1197-1204.
Crossref - Lee SM, Kang WS, Cho AR, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123-127.
Crossref - Raven J, Wurie H, Witter S. Health workers’ experiences of coping with the Ebola epidemic in Sierra Leone’s health system: a qualitative study. BMC Health Serv Res. 2018;18(1):251.
Crossref - Bryant RA. Acute Stress Disorder as a Predictor of Posttraumatic Stress Disorder. J Clin Psychiatry. 2010;72(2):233-239.
Crossref - Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38(3):192-195.
Crossref - Wu K, Wei X. Analysis of Psychological and Sleep Status and Exercise Rehabilitation of Front-Line Clinical Staff in the Fight Against COVID-19 in China. Med Sci Monit Basic Res. 2020;26:e924085.
Crossref - Hurst KT, Ballard ED, Anderson GE, et al. The mental health impact of contact with COVID-19 patients on healthcare workers in the United States. Psychiatry Res. 2022;308:114359.
Crossref - Juan Y, Yuanyuan C, Qiuxiang Y, et al. Psychological distress surveillance and related impact analysis of hospital staff during the COVID-19 epidemic in Chongqing, China. Compr Psychiatry. 2020;103:152198.
Crossref - Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, Rossi A. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Network Open. 2020;3(5): e2010185.
Crossref
© The Author(s) 2024. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.