ISSN: 0973-7510
E-ISSN: 2581-690X
The current work suggested the occurrence of blaNDM-1 gene among Klebsiella pneumoniae recovered from surface waters of the Al-Hillah River. Between January and April 2015, water samples (101) were taken from seven different area of the Al-Hillah River, Babylon province, Iraq. K.pneumoniae was reported in percentage of 35 (34.6%). The antibiotics susceptibility profile of K.pneumoniae was determined with disk diffusion assay. The most common resistance was detected for penicillins agents (ampicillin and cloxacillin) with 20(57.14%) and 17(48.57%) resistance rate, respectively. Two isolates of K.pneumoniae were carbapenem-resistant. Phenotypic screening of metallo β-lactamase detection was carried out using imipenem–EDTA double disk synergy test for carbapenem resistant isolates, 2(100%) isolates with positive result. Conventional Polymerase Chain Reaction (PCR) test was used for detection NDM-1 beta-lactamase, 1 (50%) K.pneumoniae isolate harboring this gene.
Carbapenem Resistance, Klebsiella pneumoniae, blaNDM-1 Gene, PCR, River Water
Resistant to antibiotics among bacteria has been recognized a universal risk to public and animal health globally. Aquatic system is vital habitats for pathogenic bacteria and a main route for circulation and transmission of antibiotic resistance genes in nature originating from different sources such as runoff from agricultural areas, hospital waste and domestic discharge.1-3 The greater risk for human and environmental health is the migration of antibiotic resistance genes from surrounding environment to human and animal bacterial pathogens.4-6
New Delhi metallo-beta-lactamase (NDM) is a recently described plasmid-borne carbapenemase gene belong to molecular class B beta-lactamase which readily transferred between bacteria and can lead to extreme drug-resistant phenotypes.7-9 First outbreak due to K. pneumoniae ST11producing NDM-1gene during the COVID-19 Pandemic has been particularly detected in human cases of infection in a Portuguese Hospital Centre.10 Other report achieved by Ebomah and Okoh11 identified K. pneumoniae harboring blaNDM-1 and blaKPC from various environmental niches like farm soil in the eastern Cape Province, South Africa. Multi-drug resistant Enterobacteriaceae carrying NDM-1gene have been recognized worldwide, with many cases linked to international travel and tourism.12-14
Our study aimed to provide insights on the potential the occurrence of Klebsiella pneumoniae obtained from waters of Al- Hillah river, detect resistant profiles of all isolates, determine carbapenems resistance profiles, as well as to detect blaNDM-1 gene by available phenotypic test and by conventional Polymerase Chain Reaction (PCR) assay among bacteria which resist carbapenem antibiotics.
Sampling
This study was employed from the beginning of January to the end of April 2015, surface water samples (101) were taken from seven selected sampling sites of the Al- Hillah River. It’s the main river in Babylon province, Iraq which can be used for agricultural process and as a drinking waters for animals. The sites of this study located near by each of the following region: Ancient Babylon city, Al-Wardia region, Nationality office, Bab Al-Hussein region, Al-Attba street, Al-Farisi region and Al-Aifar region. Samples were placed on sterile glass bottles, then transported to the laboratory unit (college of sciences for women, Babylon university) by ice box for immediate processing and analysis.
Processing of Samples and Microbiological Analysis
Water samples were concentrated by filtration onto a sterile filter membrane (0.22 μm) (Millipore, Difco, USA). From each dilution (ten-fold), 0.1 ml was spread on plate count agar, then incubated at 37°C for 24-48 hrs under aerobic conditions.15,16 Following incubation, bacterial colonies were sub-cultured onto different selective and enrichment media. Bacterial identification was carried out using standard biochemical and microbiological tests as described previously.17-19
Antimicrobial Assay
The identified K. pneumoniae isolates were assessed for antibiotics agents using disc diffusion test (Kirby-Bauer) on plates of Mueller- Hinton agar (Oxiod, England)20. Twelve agents were selected: ampicillin (AMP), cloxacillin (OX), amoxicillin-clavulanic acid (AMC), cefotaxime(CTX), cefoxitin (FOX), cefaclor (CF), cefprozil (CPR), imipenem (IMP), meropenem (MEM), amikacin (AK), ciprofloxacin (CIP) and norfloxacin (NOR). Diameters of inhibition zones were measured and classified as susceptible, intermediate and resistance in accordance with guidelines of the Clinical and Laboratory Standards Institute (CLSI).21 For quality control, standard strain, Escherichia coli ATCC 25922 (University of Kufa, College of Medicine) was employed.
Phenotypic Assay for Metallo Beta-Lactamase (MBL) Detection
MBLs K. pneumoniae producer was detected by phenotypic, imipenem – EDTA double disk synergy test.22
Molecular Characterization of blaNDM-1 Gene
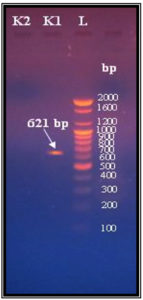
The modified method of Pospiech and Neuman (1995)23 was used to extract DNA of pure K. pneumoniae isolates and kept at -20°C. Conventional PCR technique was used for amplification of blaNDM-1 gene with specific sets of primers (Bioneer, Korea) NDM-1/F (5—GGT TTG GCG ATC TGG TTTTC -3-) and NDM-1/R (5—CGGAATGGCTCATCACGATC -3-) (621bp). The final volume of 25 µl reaction mixture contained 5µl of DNA extract,12.5 µl of Go Taq Green Master Mix 2X (Promega, USA), 2.5 µl of each primer and 2.5 µl nuclease-free water. PCR conditions included: 1 min initial denaturation at 94°C, 30 cycles of 1 min denaturation at 94°C, 1 min annealing at 55°C and 2 min extension at 72°C followed by 10 min final extension step at 72°C24,25. Electrophoresis of the product was resolved on a 1.5% agarose gel stained with ethidium bromide, then the gel was observed using UV-Transilluminator for photo-documentation.
Results identified 35/101(34.6%) isolates positive for K. pneumoniae in river waters (Table 1). Abd Al-Kareem et al.26 proved the occurrence of 40 K. pneumoniae isolates from surface water of Tigris River in Baghdad city, Iraq. Our finding also consistent with the report detected by Ebomah and Okoh11 who document 32 isolates as K. pneumoniae recovered from surface waters in the Eastern Cape Province, South Africa. Prevalence of K. pneumoniae in river water, Malaysia was (69%).27 Another study in Hillah city recorded the occurrence of same bacteria in various clinical and environmental specimens.28,29
Table (1):
Frequency of K.pneumoniae obtained from Al- Hillah river waters according to sampling sites.
Sampling location (near by) |
Samples No. |
No. (%) of isolates positive for K.pneumoniae |
|---|---|---|
Ancient Babylon city |
10 |
0 |
Al-Wardia region |
8 |
0 |
Nationality office |
6 |
0 |
Bab Al-Hussein region |
14 |
5(5.0%) |
Al-Attba street |
30 |
14(13.8%) |
Al-Farisi region |
13 |
7(6.9%) |
Al-Aifar region |
20 |
9(8.9%) |
Total |
101 |
35(34.6%) |
The existence of K. pneumoniae in surface river water may be attributed to contamination of Al- Hillah River by different sources like discharge of hospitals mainly Babylon Teaching Hospital for Maternity and Pediatric, swimming of animals and discharge their wastes directly into river stream, runoff from agricultural areas, industrial effluents. Additionally, Hillah laboratories released their waste products into these waters which stimulate the proliferation and dissemination of pan-resistant strains and even evolve various mechanisms of resistance and pathogens.
Bacterial resistance to antimicrobial agents was ancient which can occur under selective pressure. However, due to the inappropriate prescription and massive use of antibiotics in medical therapy, agriculture and aquaculture, resistant bacteria have become a serious threat worldwide.30,31 Susceptibility testing of bacterial isolates showed that most resistant agent was the penicillins antibiotics (ampicillin and cloxacillin) with 20(57.14%), 17(48.57%) resistance rate, respectively. Lihan et al.32 recorded (31.6%) resistance rate for penicillin antibiotic by bacteria including K. pneumoniae in recreational river water of a community resort in Baram, Sarawak, Malysian, Barneo.
However, penems (meropenem and imipenem) antibiotics displayed lower rates of resistant with 2(5.71%) for each, (Table 2). Bedi et al.33 detect resistance to carbapenem among 1 K. pneumoniae isolate obtained from stagnant water of Delhi\NCR.
Table (2):
Resistance profile of all 35 K.pneumoniae isolated from surface river waters.
| Antibiotic class | Agent tested | Resistant K.pneumoniae isolates No. (%) |
|---|---|---|
| Penicillins | ampicillin | 20(57.14) |
| cloxacillin | 17(48.57) | |
| β–lactams⁄β-lactamase inhibitor combinations | amoxicillin-clavulanic acid | 18(51.42) |
| Cephems | cefotaxime | 16(45.71) |
| cefoxitin | 16(45.71) | |
| cefaclor | 13(37.14) | |
| cefprozil | 13(37.14) | |
| Aminoglycosides | amikacin | 9(25.71) |
| Penems | imipenem | 2(5.71) |
| meropenem | 2(5.71) | |
| Quinolones | ciprofloxacin | 8(22.85) |
| norfloxacin | 14(40) |
All 2(100%) K. pneumoniae with resistant to carbapenem were positive for phenotypic MBL assay using the imipenem – EDTA double disk synergy test. Local study on Hillah River waters achieved by Abbas34 proved 2(66.7%) K. pneumoniae as MBL producers by this method. Shah and Zharh2 identified all (100%) meropenem resistant K. pneumoniae isolates as MBL producers.
The molecular screening of NDM-1 gene was performed using PCR technique on the two K. pneumoniae with resistant to carbapenem, the blaNDM-1 gene was detected in 1(50%) isolate only (Figure). Ahammad et al.35 documented the presence of blaNDM-1 gene among coliform bacteria from Ganges river. Shah and Zahra2 characterized 43 meropenem resistant bacteria from different water samples of which 3 K. pneumoniae isolates were harbored this gene in Islamabad, Pakistan.
This study report the finding of metallo beta lactamase of NDM-1 type containing K. pneumoniae in water samples from the Al-Hillah River. The presence of such highly resistant bacteria in water samples focus attention on the need to accelerate strategies to limit the emergence and spread of resistant organisms.
ACKNOWLEDGMENTS
I would like to acknowledge all people who provide assistance and cooperation to achieve this work.
FUNDING
None.
DATA AVAILABILITY
All datasets generated or analyzed during this study are included in the manuscript.
ETHICS STATEMENT
Not applicable.
- Martinez JL. Antibiotics and antibiotic resistance genes in natural environments. Science. 2008;321(5887):365-367.
Crossref - Shah TW, Zahra R. Screening of environment water for the presence of blaNDM-1 Gene containing microorgansims. J Coll Phys Surg Pak. 2014;24(9):695-697.
- AsfawT, Genetu D, Shenkute D. High burden of antibiotic-resistant bacteria from wastewater in Ethiopia: A systematic review. Risk Manag Health Pol. 2020;13:3003-3011.
Crossref - Kruse H. Indirect transfer of antibiotic resistance genes to man. Acta Vet Scand. 1999;92:59-65.
- Wegener H, Aurestrup F, Gemer-Smidt P, Bager F. Transfer of resistant bacteria from animal to man. Acta Ret Sand. 1999;92:51-57.
- Adelowo OO, Ikhimiukor OO, Knecht C, et al. A survey of extended-spectrum beta-lactamase producing Enterobacteriaceae in urban wetlands in southwestern Nigeria as a step towards generating prevalence maps of antimicrobial resistance. PLoS ONE. 2020;15(3):e0229451.
Crossref - Pitout JD, Laupland KB. Extended spectrum beta lactamase-producing Enterobacteriaceae: An emerging public-health concern. Lancet Infect Dis. 2008;8(3):159-166.
Crossref - Krishna B. New Delhi metallo-beta-lactamases: a wake-up call for microbiologicals. Indian J Med Microbiol. 2010;28(3):265-266.
Crossref - Nielsen JB, Hamsen F, Littaner P, Sehonning K, Hammerun AM. An-NDM-1 producing Escherichia coli obtained in Denmark has a genetic profile similar to an NDM-1 producing Escherichia coli isolate from the UK. J Antimicrob Chemother. 2012;67(8):2049-2051.
Crossref - Mendes G, Ramalho JF, Duarte A, et al. First outbreak of NDM-1-producing Klebsiella pneumoniae ST11 in a Portuguese Hospital Centre during the COVID-19 Pandemic. Microorganisms. 2022;10(2):251.
Crossref - Ebomah KE, Okoh AI. Detection of carbapenem-resistance genes in Klebsiella species recovered from selected environmental niches in the Eastern Cape Province, South Africa. Antibiotics. 2020;9(7):425.
Crossref - Yong D, Toleman MA, Giske CG, et al. Characterization of a new metallo-beta-lactamase gene, blaNDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother. 2009;53(12):5046-5054.
Crossref - Kumarasamy KK, Toleman MA, Walsh TR, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: A molecular, biological, and epidemiological study. Lancet Infect Dis. 2010;10(9):597−602.
Crossref - Chen LH, Wilson ME. The globalization of healthcare: Implications of medical tourism for the infectious disease. Clin Infect Dis. 2013;57(12):1752−1759.
Crossref - Grilich D, Poirel L, Nordman P. Novel ambler class A carbapenem-hydrolyzing β-lactamase from a Pseudomonas fluorescens isolate from the Seine River, Paris, France. Antimicrob Agents Chemother. 2010;54(1):328-332.
Crossref - Moges F, Endris M, Belyhun Y, Worku W. Isolation and characterization of multiple drug resistance bacterial pathogens from waste water in hospital and non-hospital environments, Northwest Ethiopia. BMC Res Notes. 2014;7:215-221.
Crossref - Holt JG, Krieg NR, Sneath HA, Stanley JT, Williams ST. Bergeys manual of determinative bacteriology. 9th. Ed., Baltimore; Wiliams and Wilkins, USA. 1994.
- Collee JG, Fraser AG, Marmiom BP, Simmon A. Mackie and McCarteny Practical Medical Microbiology. 4th ed. Churchill Livingstone Inc., USA. 1996.
- MacFaddin JF. Biochemical tests for identification of medical bacteria. 3rd ed. Lippincott Williams and Wilkins, USA. 2000.
- Bauer AW, Kirby WM, Sherris JC, Track M. Antibiotic susceptibility testing by standardized single disc method. Am J Clin Pathol. 1966;45(4):493-496.
Crossref - Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing. CLSI Supplement M100S.26th ed.Wayne,PA. 2016.
- Lee K, Lim YS, Yong, Yum JH, Chong Y.Evaluation of the Hodge test and the imipenem-EDTA double-disk synergy test for differentiating metallo-β- lactamase- producing isolates of Pseudomonas spp. and Acinetobacter spp. J Clin Microbiol. 2003;41(10):4623-4629.
Crossref - Pospiech T, Neumann J. In genomic DNA isolation Kieser eds. John Innes Center. Norwich NR4 7UH. U.K. 1995.
- Nordmman P, Poril L, Carrer A, Toleman MA, Walsh TR. How to detect the NDM-1 producers. J Clin Microbiol. 2011;49(2):718-721.
- Li B, Yi Y, Wang Q, et al. Analysis of drug resistance determinants in Klebsiella pneumoniae isolates from a tertiary – care hospital in Beijing, China. Plos One. 2012;7(7):e42280.
Crossref - Abd Al-Kareem AF, Al-Arajy KH, Jassim KA. Prevalence of CTX-M gene in Klebsiella pneumoniae isolated from surface water of Tigris river within Baghdad province. Adv Life Sci Technol. 2015;30:15-19.
- Barati A, Ghaderpour A, Chew L, et al. Isolation and characterization of aquatic-borne Klebsiella pneumoniae from Tropical Estuaries in Malaysia. Int J Environ Res Public Health. 2016;13(4):426.
Crossref - Al-Charrakh AH, Yousif SY, Al-Janabi HS.Ocurrence and detection of extended spectrum β-lactamases in Klebsiella isolates in Hilla, Iraq. Afri J Biotechnol. 2011;10(4):657-665.
- Abbas FM. Prevalence of transferable OXA-1 β-lactamase associated with carbapenem-resistant Klebsiella pneumoniae isolates in Iraq. J Pure Appl Microbiol. 2021;15(2):877-882.
Crossref - De Oliveira DV, Carvalho T, Medeiros AW, Frazzon APG, van der Sand ST. β -lactam resistance genes in Gram negative bacteria isolated from stream in Porto Alegre. J Adv Sci Res. 2015;6(3):19-24.
- Aslam B, Wang W, Arshad MI, et al.Antibiotic resistance: a rundown of a global crisis. Infect Drug Resis. 2018;11:1645-1658.
Crossref - Lihan K, Tian PK, Chiew TS, et al. The distribution and characterictics of bacteria in recreational river water of a community resort in Baram, Sarawak, Malysian, Barneo. Int Food Res J. 2017;24(5)2238-2245.
- Bedi N, Bansal A, Giand R. Pattern of carbapenem resistance among bacterial population in various water bodies of Delhi\NCR. Int J Pharma Bio Sci. 2017;8(3):7-11.
Crossref - Abbas FM.Prevalence and characterization of Escherichia coli and Klebsiella spp. isolated from Hilla river water. J Inter Acad Res Mutidisc. 2015;3:174-181.
- Ahammad ZS, Sreekrishnan TR, Hands CL, Knapp W, Graham DW. Increased waterborne blaNDM-1 resistance gene abundances associated with seasonal human pilgrimages to the upper Ganges river. Environ Sci Technol. 2014;48(5):3014-3020.
Crossref
© The Author(s) 2022. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.