ISSN: 0973-7510
E-ISSN: 2581-690X
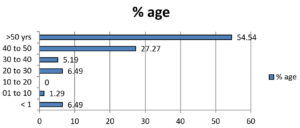
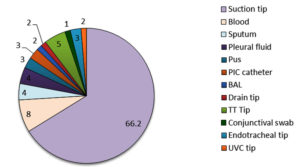
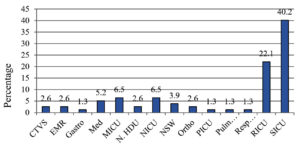
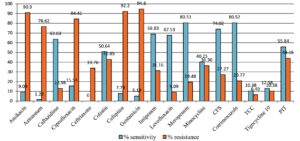
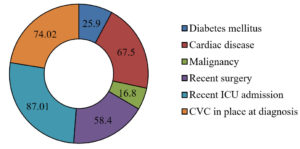
Achromobacter xylosoxidans is an emerging nosocomial pathogen which is commonly found in the environment. In hospital settings, especially in ICU, it can be a cause of nosocomial infection. It is commonly found in the humidifiers in ICU settings and it is also commonly associated with the immunocompromised state of patient having comorbidities. The objective of the study was to study the prevalence of Achromobacter xylosoxidans and its antimicrobial sensitivity pattern. The Retrospective analysis was done of the culture reports positive for Achromobacter xylosoxidans by VITEK 2 method and its Antimicrobial sensitivity pattern was analysed from the period of September 2021 to February 2023.The maximum (54.54%) infection was seen in the age group >50 years. The maximum number (66.2%) of Achromobacter xylosoxidans were isolated from Suction tip, followed by blood (8%) and Tracheal Tip (5%). Surgical ICU contributed to the maximum number of infections i.e. 40.2%, followed by Respiratory ICU (22.1%). Maximum sensitivity was seen for Cotrimoxazole and Meropenem (around 80%), followed by Cefoperazone-Sulbactam (74%), Imipenem, Levofloxacin, Ceftazidime (around 65%). The sensitivity was minimal for Ceftriaxone (0%), Aztreonam (1.3%), and Gentamicin (5.2%). The most common risk factors/ comorbidities associated with Achromobacter infections was recent ICU admission (87.01%). The antibiotic sensitivity trends to all the antibiotics used, declined from 2021 to 2022. The antibiotic of choice to our conclusion is Cotrimoxazole, followed by Piperacillin-Tazobactam. Colistin should be kept as a reserve drug for the last resort treatment. The bacteria should not be ignored as it can lead to various opportunistic infections in immunocompromised patients, causing hindrance in the treatment.
Achromobacter xylosoxidans, Nosocomial Pathogen, VITEK 2 Method, Infections, Opportunistic Infections, Antimicrobial Susceptibility
Achromobacter xylosoxidans are gram negative rod, which are widely distributed in the environment in water and soil and becoming an emerging cause of health care associated infections. It is aerobic, motile, catalase and oxidase positive, non-fermenting bacteria.1 Previously classified as Alcaligenes xylosoxidans, it has recently been renamed as Achromobacter xylosoxidans.2 Genus Achromobacter comprises of 19 species.3 Out of these, 15 species have been isolated from clinical specimens till date.1 A. xylosoxidans is the most common species recovered from clinical samples, including those derived from persons with cystic fibrosis followed by Achromobacter ruhlandii.4-8 It is considered as a cause of opportunistic infections in humans which can manifest as pulmonary infections like chronic respiratory infections. Also, the Extra- pulmonary manifestations are seen as sepsis, bacteraemia, endophthalmitis, keratoconjunctivitis, catheter associated bloodstream infection, endocarditis, pneumonia, meningitis, and peritonitis and even as device associated infections.9 Although Pseudomonas aeruginosa and Staphylococcus aureus are the most common bacteria causing Cystic fibrosis, pulmonary disease, over the last two decades some more pathogens have been identified in patients with CF, which includes Stenotrophomonas maltophilia, nontuberculous mycobacteria (NTM), and Achromobacter species.10 Being in the category of opportunistic infections, it is most commonly associated with the immunosuppressed persons who have co-morbidities and also the patients with malignancies.11,12 A. xylosoxidanshas the capability of forming biofilms in water systems and contaminating solutions.13-15 The have multidrug resistance to various antibiotics due to their large genome which is rich in C-G sequence, their intrinsic resistance to arsenic and ability to degrade aromatic compounds.16 The intrinsic resistance may also attribute to the various mechanisms, including chromosomally encoded efflux pumps and b-lactamases which reduce the susceptibility of A. xylosoxidans to various antibiotics like carbapenems, cephalosporins, and fluoroquinolones.17 Also, resistance to carbapenems is conferred due to acquisition of metallo-b-lactamases via mobile genetic elements.18 Hence, they are difficult to treatbecause they are intrinsically resistant to a wide range of antimicrobial agents and have the potential to develop the acquired resistance mechanisms in future. Thus, the eradication of Achromobacter sp. can be difficult. As a result, this can lead to chronic infection.2 Varied case-fatality rates have been reported, which varies from 3% to 80 %, more in number for neonatal infections.19
As Achromobacter is an emerging bacterium in health care settings, it is important to know the trend in prevalence and Antimicrobial Sensitivity pattern in Health care settings. Bacteraemia due to A. xylosoxidans can be a serious complication among hospitalized patients. Therefore, we conducted a retrospective study to evaluate the prevalence and trends of Achromobacter xylosoxidans in clinical specimens and the trend in its sensitivity pattern.
The study was conducted retrospectively in a 1500 bedded tertiary care hospital in North India. The study included samples from all age groups that tested positive for Achromobacter xylosoxidans. Ethical clearance was taken by the institutional Clinical Ethics Committee. The cases were identified by the computerized database of VITEK system in the Microbiology department. Samples (like urine, ET Secretion, blood, Suction Tip, sputum, conjunctival swab, etc) from all the age groups which tested positive for Achromobacter xylosoxidans were included in this study. Samples positive for the bacteria other than Achromobacter xylosoxidans were excluded from the study.
The samples were processed according to the protocol followed in the Microbiology Lab. Blood samples were subjected to aerobic culture using BACT/ALERT 3D microbial detection system (bioMerieux India Private Limited). The blood culture bottles which beeped positive were subjected to preliminary microscopic examination of Gram-stain. Subcultures were also performed from these bottles on blood and MacConkey agar plates at 48hrs and 72 hrs which were incubated aerobically at 37°C overnight. The plates were kept incubated in BACT/ALERT upto day 5, before reporting it negative (In case there was no beep). Antibiotic susceptibility testing of bacterial isolates was performed using Vitek 2 compact automated machine, the results of which were interpreted as per Clinical and Laboratory Standards Institute guidelines. American Type Culture Collection control strains were used to ensure the quality of each procedure.
The samples other than Blood were processed in VITEK 2 after processing in the Culture media like Blood Agar, Maconkey agar, Chocolate agar, CLED agar (In case of Urine samples).
This retrospective study was conducted from September 2021 to February 2023 in a tertiary care hospital in North India. 79 samples were positive for Achromobacter xylosoxidans out of the total samples received (of all the ages) in the microbiology lab for culture. Figure 1 shows that the maximum age group from which the sample is received in the lab is the group belonging to >50 years of age, followed by 40-50 years of age. There were no samples from 10-20 years of age group. The maximum number (66.2%) of Achromobacter xylosoxidans were isolated from Suction tip, followed by blood (8%) and Tracheal Tip (5%). Whereas, only 1 % of samples were detected positive from conjunctival swab for Achromobacter xylosoxidans (Figure 2). The samples in the central laboratory of the tertiary care centre are received from various departments and wards. Figure 3 shows that out of the 79 isolates of Achromobacter xylosoxidans, maximum (40.2 %) were received from Surgical ICU (SICU), followed by Respiratory ICU (RICU) (22.1%). From rest of the departments, the percentage of isolation of Achromobacter xylosoxidans was very few ranging from 1.3% to 6.5%. As depicted in Figure 4, Sensitivity of Achromobacter xylosoxidans is maximally seen for Cotrimoxazole and Meropenem (around 80%), followed by Cefoperazone-Sulbactum (74%), Imipenem, Levofloxacin, Ceftazidime (around 65%). The sensitivity is minimal for Ceftriaxone (0%), Aztreonam (1.3%), Gentamicin (5.2%). In Figure 5, it is shown that amongst 79 isolates of Achromobacter xylosoxidans, maximum i.e. 87% were associated with the recent ICU admission. 74 % had the CVC in place, 67.5% of the patients were associated with the Cardiac disease and 58.4 % had recent surgery. Table and Figure 6 shows the decreasing trends in terms of sensitivity pattern from 2021 to 2022. The Sensitivity for all the antibiotics has been decreased in 2022 as compared to 2021.
Table:
Pattern in 2021 and 2022
2021( %) |
2022 (%) |
|
|---|---|---|
Amikacin |
14.28 |
4.76 |
Aztreonam |
0 |
1.58 |
Ceftazidime |
50 |
66.66 |
Ciprofloxacin |
14.28 |
15.87 |
Ceftriaxone |
0 |
0 |
Colistin |
78.57 |
46.03 |
Cefepime |
14.28 |
4.76 |
Gentamicin |
21.42 |
3.17 |
Imipenem |
85.71 |
61.90 |
Levofloxacin |
57.14 |
69.84 |
Meropenem |
85.71 |
79.36 |
Minocycline |
42.85 |
39.68 |
Cefoperazone sulbactam |
71.42 |
71.42 |
Cotrimoxazole |
85.71 |
77.77 |
Piperacillin-Tazobactum |
57.14 |
55.55 |
Tigecycline |
42.85 |
0 |
Ticarcillin-Clavulanate |
42.85 |
0 |
Figure 3. Percentage of the most common departments from where Achromobacter xylosoxidans is isolated
Achromobacter xylosoxidans which usually is an environmental contaminant, found in soil, water, etc, can exist as a normal flora in the human body over the skin and gastrointestinal tract. It is mostly associated with opportunistic infections amongst immunocompromised patients admitted in the hospitals.20 Achromobacter has many species reported.3 Achromobacter xylosoxidans was identified in all the samples in this study.
Although majority of the reports have not mentioned the predominant age for Achromobacter infections. In our study, the maximum number of cases were reported from the age group of >50 years of age. Besides this, the study done by Barragan et al. also reported the maximum infections in the mean age group of 50 years.21 This may be due to the fact that the persons in this age group are prone to have comorbidities and also have a weaker immune system.
As Achromobacter is emerging as a cause of Nosocomial infections, It has been reported from various specimens, indicating the pathology of the various systems involved. A. xylosoxidans is an opportunistic bacterium that can cause infections in various systems of the body of immunocompromised individuals. It is mostly associated with pneumonia, sepsis, meningitis and urinary tract infections in immunocompromised patients.22 In our study , we found the maximum isolation of 85% Achromobacter xylosoxidans from the respiratory samples i.e. suction tip, sputum, pleural fluid, BAL, Tracheal tip, Endotracheal tip. Suction tip being the most common with 66.2% of Achromobacter, whereas, only 15% of the non-respiratory samples reported Achromobacter. HAIs due to Achromobacter have also been reported in ocular infection.23,24 Whereas in our study, only 1% of ophthalmological specimen i.e. conjunctival swab having Achromobacter infections is reported.
In a study conducted by Aisenberg et al., it has been reported that primary bacteraemia is the most common clinical presentation amongst neutropenic patients.25 Kar et al. reported 0.57% of the Achromobacter associated bacteremia in a study conducted for one year.26 Whereas, in the present study, we found only seven (8%) of the patients with Achromobacterbacteraemia.Four out of seven patients were on peripheral vascular catheter, indicating that the cause may be inappropriate technique for blood withdrawal. The Report by Tena D et al. shows that the Urinary Tract infections (UTI) due to Achromobacter is very rare and usually is associated with the Comorbidities.27 A case report by Sari S et al. reported a case with Achromobacter UTI in a secondary kidney stone patient who was diabetic and had a history of previous surgery for right kidney stone.28 Our study followed the similar pattern in terms of Urine sample positivity for Achromobacter. In the present study, we did not found any urine sample positive for Achromobacter xylosoxidans.
Although the case reports are there regarding Achromobacter meningitis.29,30 Contrary to these studies, we had not received any CSF which was positive for Achromobacter species.
Achromobacter infections are most commonly found in the patients with compromised immune system. In our study, the most common group of people who developed Achromobacter infections were the people who had undergone recent surgery and were admitted in the ICU settings. Out of the 87% of the patients admitted in the ICU, 40.2 % developed Achromobacter infections, thus reiterating the fact that Achromobacter is most commonly a nosocomial pathogen which affects the immunocompromised persons the most.
As described in an article by Isler et al., A. xylosoxidans is intrinsically resistant to penicillins, first- and second-generation cephalosporins, ceftriaxone, cefotaxime, aztreonam, tetracycline, and aminoglycosides.4 In our study, Aztreonam and ceftriaxone were zero percent (0%) susceptible to Achromobacter. Whereas, aminoglycosides such as Amikacin and Gentamicin had shown a very low sensitivity pattern in vitro with 9% and 5% sensitivity, respectively. These results were similar to the study by Beaurelle et al. which also has reported the zero (0%) susceptibility to Aztreonam and Gentamicin, and only 13% sensitivity for Amikacin.4
The most effective agents against Achromobacter species are Trimethoprim-sulfamethoxazole, ceftazidime, piperacillin and carbapenems.31 In our study, the maximum susceptibility is seen for Cotrimoxazole (80.59%), followed by carbapenems like Meropenem (80.52%) and Imipenem with 68.83%. Sensitivity to ceftazidime (63.63%) was lower than cotrimoxazole and carbapenems. Similar to our findings, in the study done by Barragain et al., Cotrimoxazole and Ciprofloxacin were found resistant at a notable rate. Whereas, Carbapenems and piperacillin-tazobactum were sensitive in their study also as in our study.21 The sensitivity to Meropenem was higher than that of Imipenem in our study, whereas, it was vice versa in the study by Beaurelle et al. It is important to know that only 50% of the isolates were sensitive to Colistin in our study. Similar results were seen in the study done by Beaurelle et al., where only 30% of the isolates reported Colistin susceptibility.4 The reason for this may be due to the injudicious use of colistin. Since, Colistin is the last resort drug for gram negative bacteria infection, it should be kept reserved. This variation in antibiotic sensitivity or resistance can be due to the various factors like: antibiotics used in patients in primary treatment, immune status of the patients from which the sample collected, overuse or misuse of antibiotics, availability of antibiotics, etc.
Achromobacter has various species but the most common is Achromobacter xylosoxidans. Achromobacter xylosoxidansis an emerging nosocomial pathogen which is commonly found in the environment. In hospital settings, it can be a cause of nosocomial infection, specially in ICU settings as it is a common reservoir of the aquatic environment which is commonly found in the humidifiers in ICU settings and it is also commonly associated with the immunocompromised state of patient having comorbidities. As, it is a concealed cause of infection, injudicious use of antibiotics are the major cause of the multiple drug resistance against it. The antibiotic of choice to our conclusion is Cotrimoxazole, followed by Piperacillin-Tazobactum. Colistin should be kept as a reserve drug for the last resort treatment. The bacteria should not be ignored as it can lead to various opportunistic infections in immunocompromised patients, causing hindrance in the treatment.
ACKNOWLEDGMENTS
The authors would like to thank Chairman SGRRIM & HS for providing the facilities to conduct the research work.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
DR conceptualized and designed the study. RR collected the data. HN performed statistics and data analysis. MS wrote the manuscript. AP reviewed and edited the manuscript. All authors read and approved the final manuscript for publication.
FUNDING
None.
DATA AVAILABILITY
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
ETHICS STATEMENT
Not applicable.
- Isler B, Kidd TJ, Stewart AG, Harris P, Paterson DL. Achromobacter infections and treatment options. Antimicrob Agents Chemother. 2020;64(11):e1025-20.
Crossref - Lambiase A, Catania MR, del Pezzo M, et al. Achromobacter xylosoxidans respiratory tract infection in cystic fibrosis patients. Eur J Clin Microbiol Infect Dis. 2011;30:973-980.
Crossref - Dumolin C, Peeters C, Ehsani E, et al. Achromobacter veterisilvae sp. nov., from a mixed hydrogen-oxidizing bacteria enrichment reactor for microbial protein production. Int J Syst Evol Microbiol. 2019;70:530 -536.
Crossref - Beauruelle C, Lamoureux C, Mashi A, et al. In Vitro Activity of 22 Antibiotics against Achromobacter Isolates from People with Cystic Fibrosis. Are There New Therapeutic Options? Microorganisms. 2021;9(12):2473.
Crossref - Garrigos T, Neuwirth C, Chapuiset A, Bador J, Amovrex L, Collaorators. Development of a database for the rapid and accurate routine identification of Achromobacter species by matrix-assisted laser desorption/ionizationetime-of-flight mass spectrometry (MALDI-TOF MS). Clin Microbiol Infect. 27. 2021;27(1):126.e1-126.e5.
Crossref - Sahl C, Baumgarten M, Shannon O, Pahlmana L. Exoproducts of the Most Common Achromobacter Species in Cystic Fibrosis Evoke Similar Inflammatory Responses In Vitro. Microbiol Spectr. 2023;11(4).
Crossref - Veschetti L, Boaretti M, Saitta GM, et al. Achromobacter spp. prevalence and adaptation in cystic fibrosis lung infection. Microbiol Res. 2022;263:127140.
Crossref - Cobian Guemes AG, Le T, Rojas MI, et al. Compounding Achromobacter Phages for Therapeutic Applications. Viruses. 2023;15(8):1665.
Crossref - Chalhoub H, Kampmeier S, Kahl BC, Van Bambeke F. Role of Efflux in Antibiotic Resistance of Achromobacter xylosoxidans and Achromobacter insuavis Isolates From Patients With Cystic Fibrosis. Front Microbiol. 2022;13:762307.
Crossref - Kerem E, Orenti A, Zolin A, Annicchiarico L, Drevinek P. Clinical outcomes associated with Achromobacter species infection in people with cystic fibrosis. J Cyst Fibros. 2023;22(2):334-343.
Crossref - Swenson CE, Sadikot RT. Achromobacter Respiratory Infections. Ann Am Thorac Soc. 2015;12(2):252-258.
Crossref - Siddiqui T, Patel SS, Ghoshal U, Sahu C. Clinicomicrobiological profile of infections by Achromobacter: An emerging nosocomial pathogen in Indian hospitals. Int J App Basic Med Res. 2023;13(2):59-63.
Crossref - Marion-Sanchez K, Olive C, Platon MG, Cesarine M, Derancourt C, Pailla K. Achromobacter Xylosoxidans in Hospital Environments: Still Waters Run Deep. Trans R Soc Trop Med Hyg. 2020;114(6):470-472.
Crossref - Menetrey Q, Sorlin P, Jumas-Bilak E, Chiron R, Dupont C, Marchandin H. Achromobacter xylosoxidans and Stenotrophomonas maltophilia: Emerging Pathogens Well-Armed for Life in the Cystic Fibrosis Patients’ Lung. Genes. 2021;12(5):610.
Crossref - Isler B, Paterson DL, Harris PNA, et al. Achromobacter Species: An Emerging Cause of Community-Onset Bloodstream Infections. Microorganisms. 2022;10(7):1449.
Crossref - Majumder A, Bhattacharyya K, Bhattacharyya S, Kole SC. Arsenic tolerant, arsenite-oxidising bacterial strains in the contaminated soils of West Bengal, India. Sci Total Environ. 2013;463-464.
Crossref - Gabrielaite M, Bartell JA, Norskov-Lauritsen N, et al. Transmission and Antibiotic Resistance of Achromobacter in Cystic Fibrosis. J Clin Microbiol. 2021;59(4):e02911.
Crossref - MacDonald L, Keenan S, Di Lorenzo F, et al. Polymyxin Resistance and Heteroresistance Are Common in Clinical Isolates of Achromobacter Species and Correlate with Modifications of the Lipid A Moiety of Lipopolysaccharide. Microbiol Spectr . 2023;11(1):e03729-22.
Crossref - Pandey K, Nawtiyal S. Achromobacter: An emerging nosocomial pathogen. Int J Res Med Sci. 2019;7(8):3090-3094.
Crossref - Mudey G, Kunjalwar R, Sahu G, Mahajan SM, Meshvam S. Sepsis Due to Achromobacter xylosoxidans in a Tertiary Care Centre: Case Series. Cureus. 2023;15(7):e42052.
Crossref - Barragan EP, Perez JS, Corbella L, Orellana MA, Fernandez-Ruiz M. Achromobacter xylosoxidans bacteremia: clinical and microbiological features in a 10-year case series. Rev Esp Quimioter. 2018;31(3):268-273.
- Reddy AK, Garg P, Shah V, Gopinathan V. Clinical, microbiological profile and treatment outcome of ocular infections caused by Achromobacter xylosoxidans. Cornea. 2009;28(10):1100-1103.
Crossref - Villegas VM, Emanuelli A, Flynn HW, et al. Endophthalmitis caused by Achromobacter xylosoxidans after cataract surgery. Retina. 2014;34(3):583-586.
Crossref - Astley RA, Mursalin MH, Coburn PS, et al. Ocular Bacterial Infections: A Ten-Year Survey and Review of Causative Organisms Based on the Oklahoma Experience. Microorganisms. 2023;11(7):1802.
Crossref - Aisenberg G, Rolston KV, Safdar A. Bacteremia caused by Achromobacter and Alcaligenes species in 46 patients with cancer (1989-2003). Cancer. 2004;101(9):2134-2140.
Crossref - Kar M, Singh R, Tejan N,et al. One year experience of Achromobacter bacteremia at a tertiary care hospital in Northern India. Access Microbiology. 2023;5(9).
Crossref - Tena D, Gonzalez-Praetorius A, Perez-Balsalobre M, Sancho O, Bisquert J. Urinary tract infection due to Achromobacter xylosoxidans: Report of 9 cases. Scand J Infect Dis. 2008;40(2):84-87.
Crossref - Sary S, Yesilyurt E, Yilmaz N, Gurel A, Gurtan E, Sanal L. Achromobacter xylosoxidans infection in urinary tract in a secondary kidney stone patient: Case Report. J Surg Med. 2018;2(3):406-407.
Crossref - Orni M, Znazen M, Borni FC, Boudawara MZ. A case of meningitis due to Achromobacter xylosoxidans in a child with a polymalformative syndrome: a case report. Pan Afr Med J. 2021;39:124.
Crossref - Manckoundia P, Mazen E, Coste AS, et al. A case of meningitis due to Achromobacter xylosoxidans denitrificans 60 years after a cranial trauma. Med Sci Monit. 2011;17(6):63-65.
Crossref - Bonis, Hunter. JMM Profile: Achromobacter xylosoxidans: the cloak-and-dagger opportunist. J Med Microbiol. 2022;71(5).
Crossref
© The Author(s) 2023. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.