Monkeypox is a zoonotic infection that causes painful or pruritic dermatologic lesions on the face, trunk, limbs, genitals, and mucosal surfaces. Monkeypox cases increased exponentially in 2022, prompting the World Health Organization and the United States Department of Health and Human Services to proclaim it a public health emergency. The role of community health nurses towards monkeypox prevention and control in transmission. We searched various databases like World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), American Nurses Association (ANA), EMBASE, Web of Science, CINAHL, PubMed, and Cochrane databases were comprehensively searched. This review article focuses on the monkeypox pandemic, the transmission of the infection, vaccination and the role of healthcare workers. The healthcare role is crucial in preventing and promoting the monkeypox pandemic. These results can be consolidated when policymakers plan to increase the implementation of the healthcare worker in the face of monkeypox and future global threats.
Monkeypox, Zoonotic, Health Care Worker, Vaccination, Prevention
World health organization (WHO) proclaimed a public health emergency of international concern on July 23rd, 2022, in response to the quickly distending monkeypox crash. Monkeypox is a zoonotic disease that spreads from animals or humans with direct contact with fluid, abrasion, or wound. Human-to-human transmission occurs only when a person is in direct contact with an incubation period of 5-12 days. The exact manifestation is rashes observed all over the body area.1
In August 2022, worldwide 47.652 confirmed cases and 13 deaths were reported in 99 countries. The vaccine used as a preventive measure for monkeypox is the vaccine for smallpox which is 85% effective in preventing monkeypox.2 Monkeypox is a viral zoonosis transmitted to humans from animals and has the same symptoms as smallpox patients develop but is less severe. Smallpox was eradicated in 1980; meanwhile, the vaccination for smallpox was stopped; the new arrival of monkeypox occurred, which has been the most crucial orthopox virus in community settings.1 The first isolation and recognition of the monkeypox virus occurred from Singapore to the Danish research center while transferring sick monkeys in 1958. The first known case of the disease in a human was recognized in a young boy in the democratic republic of the Congo who was assumed to have smallpox in 1970.3
Contagious infections are one of the significant possible trouble facing the community in various public health emergencies.4 There is a great need for the requirement of healthcare personnel during health emergencies and in executing several plans to meet the challenges that can react to epidemics.5 Frontline health nurses are the essential workforce dealing with disease in various community settings. In the case of management, they play a leading role in disease prevention and surveillance.6 The nurses must be prompt enough to handle the situation during epidemic conditions such as monkeypox.
Frontline health workers should spread awareness of epidemics like monkeypox and confirm that the community is protected.7 Healthcare professionals, testing capacity, public health monitoring, safety equipment, and emergency planning resources have all been severely damaged by the global monkeypox epidemic. Monkeypox could spread uncontrollably if early detection and adequate treatment are not delivered.5
To fight the monkeypox outbreak, frontline nurses are essential in providing health education on infection management, prevention, and stigma reduction.6 However, the monkeypox outbreak strains nurses who provide first-line treatment to infected patients, much like any other pandemic or endemic. The monkeypox virus can also spread to anyone who works closely with an infected person and cannot only be transmitted from one person to another through sexual contact. As a result, the frontline health workers are anxious and agitated.7 Although caring for patients gives them a sense of fulfillment, they also feel physically and mentally uncomfortable. These include feeling unqualified for the job, witnessing patients in pain, experiencing discomfort from wearing personal protection equipment (P.P.E.) clothing, and long work hours that could harm interpersonal relationships. The administrators of healthcare facilities are forced to pay close attention to nurses and healthcare workers due to several factors, including the need for physical and mental support, welfare services, training opportunities, adoption of modern technologies, and safeguarding nurses from illness.6,7
Patients must be isolated and vulnerable skin and mucous membranes must be protected as part of the nursing management of monkeypox patients. Dehydration and loss of appetite are potential symptoms for the patient. The nurse should try to rehydrate the patient, give nutritional assistance, check vital signs, constantly monitor the patient, and keep an eye out for any complications. Additionally, the patient should wear a triple mask layer and cover as much of their skin lesions as possible to lessen the chance of coming into touch with others (e.g., long sleeves and long pants). There are no confirmed, clinically effective therapies for monkeypox disease.7 Most viral infections require supportive care, such as antipyretics and dehydration management.
Nurses are the foundation of hospitals. Nurses’ safety is essential In response to pandemics and outbreaks of monkeypox. Worldwide, there is concern about inadequate support and safety measures for nurses during severe infectious disease epidemics. An effective response to a monkeypox outbreak requires cooperation on a practical level between nurses, health organizations, and authorities. The availability of policies and practices that can be adapted is an essential aspect of minimizing nosocomial infection rates.
Review
Prevalence
There were 0.63 instances of monkeypox reported annually per 10,000 people, with notable disparities in age, location, and incident rate between the unvaccinated group (1.7/10,000) and the population who received vaccinations (0.04/10,000) per year.8
Sign and Symptoms
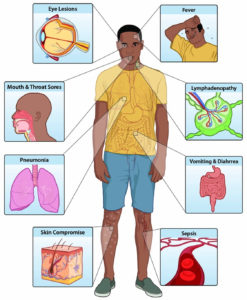
Monkeypox typically has an incubation period of 6 to 13 days, although it can occur anywhere between 5 to 21 days for symptoms to appear.3
The infection can be divided into two periods.
Fever, headache, lymphadenopathy (swelling of the lymph nodes), back discomfort, myalgia (muscle aches), and acute asthenia are the hallmarks of the invasion period, which lasts between 0 and 5 days. When compared to other infections that may initially appear similar, monkeypox is distinguishable by its lymphadenopathy (chickenpox, measles, smallpox) (Figure).1
Open access journal under a CC-BY license Contributed by Mary G. Reynolds9
Typically, the skin eruption starts one to three days after the fever appears. The face and extremities are frequently the focus of the rash rather than the trunk. In 95% of cases, it affects the face, and in 75% of cases, it affects the palms of the hands and the soles of the feet. Also impacted are the cornea, conjunctivae, genitalia, and oral mucous membranes (in 70% of cases). The progression of the rash goes from macules (flat, firm lesions) to papules (slightly raised, firm lesions), vesicles (clear fluid-filled lesions), pustules (yellowish fluid-filled lesions), and crusts that dry up and break off. Lesions can range from a few to several thousand. Lesions can merge in severe situations, causing huge amounts of skin to slough off.10
Monkeypox is typically a self-limiting illness with symptoms lasting around two to four weeks. Children are more likely to experience severe cases correlated with patient health, the extent of viral exposure, and consequences. The results could be worse due to underlying immunological inadequacies. Although smallpox immunization was protected in the past, due to the worldwide discontinuation of smallpox vaccination campaigns after the disease’s elimination, youngsters between the ages of 40 to 50 may now be more susceptible to monkeypox. Monkeypox complications can include secondary infections, bronchopneumonia, sepsis, encephalitis, and corneal disease with subsequent vision loss. The extent to which asymptomatic infection may develop is unknown.1 Monkeypox case fatality rates have historically ranged from 0 to 11% in the general population, with small children being more susceptible. The case mortality rate has recently ranged at 3-6%.1
Vaccination
Numerous observational studies have shown that the smallpox vaccine is around 85% effective at preventing monkeypox. There may be a milder sickness as a result of previous smallpox vaccination.11 A scar on the upper arm is typically proof of prior smallpox immunization. Public access to the first-generation (original) smallpox vaccinations has ended. Some laboratory or healthcare employees may have a more current smallpox vaccination to safeguard them from orthopoxvirus exposure at work. In 2019, an even more recent immunization based on the Ankara strain of the modified attenuated vaccinia virus was authorized to protect monkeypox. This two-dose vaccine is only partially available. Due to cross-protection for the immune response to the orthopoxvirus, smallpox and monkeypox vaccines are based on the vaccinia virus.10
Diagnosis
The medical practitioner diagnosed monkeypox by taking a swab from the part of the rash. Physicians should be able to recognize rash-producing illnesses like smallpox and measles and screen for STIs like HIV, syphilis, and other factors.12
Prevention
Primary prevention for monkeypox is to increase public awareness of risk factors and symptoms and educate people regarding actions to reduce their exposure to the virus. Currently, research has been conducted for the prevention and control of monkeypox to determine the feasibility and appropriateness of vaccination.7 Some countries are developing policies to provide vaccines to frontline workers such as laboratory personnel, rapid response teams, and health workers.9
Reducing the risk of human-to-human transmission
During the pandemic, instant identification and survey are crucial to recognizing new cases. People with infection need to be isolated during the outbreak of human monkeypox, due to which monkeypox infection can spread rapidly. Frontline workers are at higher risk of infection. Standard infection control must be taken by healthcare workers while caring for and handling the specimens of patients diagnosed with monkeypox. Vaccinated staff against smallpox can only care for the patient with monkeypox.1
The well-qualified and experienced staff in fully equipped laboratories can handle the samples and specimens taken from animals and individuals suspected of monkeypox infection. According to guidelines given by WHO for transporting infectious substances, the specimen should be prepared with triple packaging for transportation.5
Several cases of monkeypox without direct contact with infectious people were found in May 2022 in non-endemic countries. The root of the occurrence of monkeypox has been investigated as well as several modes of transmission are needed to be closed to safeguard the community people.8
Reducing the risk of zoonotic transmission
Many human infections have been transmitted directly or from animals to humans. When contacting sick wild animals, they should use protected equipment and handle the blood; meat should be avoided without using protective equipment. Before eating any animal, meat should be cooked thoroughly.13
Preventing monkeypox through restrictions on animal trade
Many countries made rules and regulations for the restriction of rodents. Instant quarantine should be done for animals with monkeypox infection and placed in isolation from other animals. If the animals come into contact with an infected animal, they should be isolated and assessed over 30 days for monkeypox symptoms and need to handle with precautions.10
Role of community health nurse
The integrated part of community health care activities is community health nursing. Community health nursing deals with the group of community people to improve their quality of life and helps solve the various problems that cause susceptibility to health problems and risks.14 There is a great need in today’s community for complexity and adapting advanced technology. To face the existing challenges, the community health nurse must apply a holistic and integrated approach.15
Several types of research revealed that in a pandemic like a monkeypox crisis, nurses have experience and understanding regarding several aspects of the disease, like isolation wards, casualty, and ICU. These are reviews outside the Community health care, but due to this crisis, the community faces many challenges, and to overcome these challenges, the people require community health nurses.16 During a situational crisis like a pandemic, community health nurses need competencies that could improve the skills nurses to overcome the situation. The C.H.N. has made community people more attentive to the fight against chronic disease and disease threats.17
Nursing Approach
Nurses played an important role in community health crises and were seriously influenced during the monkeypox epidemic. Nurses are vital during the pandemic as it is very difficult to use diverse healthcare systems to respond to emergencies in different content of care.18
Nurses are in great need of personal protective equipment, but in the pandemic situation, the availability of P.P.E. is very low and staff couldn’t get through, which staff faces many challenges like less work satisfaction and increased risk of infection among the staff.19
During a pandemic, the nurses reported many problems like the inability to communicate with families and relatives due to the P.P.E and isolation and the need for human resource allocation and CNE to develop new skills and become competent. The crucial aspect of nursing during the monkeypox involves personal care.19 Personal care in the aspects of nursing includes environmental care. Also, it can be affected during emergencies which deteriorates the prognosis and satisfaction with care.20
Precautions for Preventing Monkeypox Virus Transmission
If a patient seeking care is suspected of having a monkeypox infection, further infection control procedures should be implemented in addition to Standard Precautions Personnel responsible for infection prevention and control should be notified immediately. Activities that may cause dried material from lesions to resuspend (e.g., use of portable fans, dry dusting, sweeping, vacuuming) should be avoided.11
Patient Placement
Whether suspected or confirmed, a patient with monkeypox infection should be treated in a single-person room; no additional air handling is necessary. The door should always be kept shut (if safe to do so). The patient needs to have a committed bathroom. Shipping and acts done by the patient out of doors must be restricted to medically essential purposes. The patient should use well-fitting reservoir control (e.g., medical mask) when transferred out of the room and clothed with a sheet or gown if exposed to skin contusion. Several procedures like intubation and extubation probably transmit oral secretions that must be carried out in an isolated airborne area.11
Personal Protective Equipment (P.P.E.)
Healthcare professionals use gowns, gloves, and eye protection like goggles or a face shield that protect the front and side of the face) while entering the patient’s room, As per NIOSH- approved particulate inhalator equipped with N95 respirators or more.8
Environmental Infection Control
Standard practices to be performed while handling the soiled laundry, like bedding, towels, personal clothing, and contusion material, must be avoided during contact at the time of laundry. Soiled laundry needs to be smoothly and instantly contained in a suitable laundry bag and not handled, due to which the infectious substance may scatter.21 Activities like dry dust, seeping, and vacuum cleaning should be avoided. A wet cleaning method has been chosen. Regular procedures need to be carried out for managing food service items.9
Duration of Isolation Precautions for Patients with Suspected or Confirmed Monkeypox Infection
Patients with monkeypox infection need to have isolation precautions until the monkeypox infection is eliminated. The monkeypox carrier will be isolated unless all abrasions are crusted, and a new healthy skin layer is formed beneath. Discontinuation of the isolation depends on the jurisdiction in a healthcare setup, which should have a consultation with local and state health departments.10
Management of Patients with a Monkeypox Virus Exposure
Patients in healthcare setup who has monkeypox virus exposure but do not have symptoms should not be isolated but to be monitored. Assess the patients for monkeypox signs and symptoms, including skin examination at least daily for about 21 days after the last exposure. Community guidelines to be adapted for risk assessment and management of patients after monkeypox exposure dependent on the nature and location of patients.9,10,19
During the 21-day monitoring period
If any rash occurs on the patient’s body, they should be placed on factual isolation precautions until the rashes are assessed, testing has been performed, and the findings are available. Other than rashes, if symptoms are present, the patients need to be isolated for about five days and twenty-one days as a monitoring period for developing new symptoms.14
If the patients do not have any new symptoms for the past five days and skin and oral assessment reveal no lesion or rash, the isolation precaution should be discontinued. Isolation precautions could be discontinued if monkeypox has been treated. If patients develop new symptoms during 21days, so patients need to be isolated again for five days.1,10,11,13
There is no monkeypox transmission by blood transfusion, organ transplantation, implantation, infusion, or transfer of human cells, tissues, or cells. Some precautionary measures to be followed include not donating blood, cells, tissues, breast milk, or semen. Patients exposed to monkeypox symptoms but do not have any symptoms and no evidence of monkeypox can donate organs with proper appropriate precaution.9
Several patients cannot tell the onset of symptoms, e.g., a newborn or patients with delirium. So patients should be isolated until they say to the commencement of symptoms like delirium resolution or be isolated after the last exposure. Decisions have to be taken to isolate the patients who can’t communicate the course of symptoms and thus risk transmitting the other patient’s unit like in the immunocompromised person.6,15
Visitation
Visitors should be minimized to patients with monkeypox infection, like parents of a child or spouse. Decisions are to be taken based on the visitor’s stay or sleep in the patient’s room, age, ability to promote themselves and visitor comply infection prevention, the already the visitor risk, and many other aspects. Visitors with communicable diseases need not visit patients with monkeypox symptoms to minimize the risk of cross-infection and the transmission of infection.11
After the covid-19 pandemic, monkeypox was creating crises in the world. Using a mask and close contact with the infected person can prevent monkeypox. The role of health care in the pandemic plays a crucial role in controlling and preventing the monkeypox pandemic. Healthcare plays a vital role in monkeypox management by providing complete services, mechanization, family nursing services, community delegation, and teamwork over several programs and regions. These results can be consolidated when policymakers plan to increase healthcare providers’ implementation in the face of monkeypox and future global threats. Studies are in great need to reduce the health care provider as an essential component in managing monkeypox and preventing several health problems in community settings.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORS’ CONTRIBUTION
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
FUNDING
None.
ETHICS STATEMENT
Not applicable.
AVAILABILITY OF DATA
Not applicable.
- WHO. Monkeypox. https://www.who.int/news-room/fact-sheets/detail/monkeypox. Accessed 2022-09-16.
- Ibrahim PK, Abdulrahman DS, Ali HM, et al. The 2022 Monkeypox Outbreak – Special Attention to Nurses’ Protection Should Be a Top Priority. Ann Med Surg (Lond). 2022;82:104615.
Crossref - Moore MJ, Rathish B, Zahra F. Monkeypox. In StatPearls; StatPearls Publishing: Treasure Island (FL). 2022.
- Ahmed SK, M-Amin HI, Abdulqadir SO, et al. Timely Mental Health Care for the 2022 Novel Monkeypox Outbreak Is Urgently Needed. Ann Med Surg (Lond). 2022;82:104579.
Crossref - Awan MAE, Waseem M, Sahito AF, et al. Monkeypox Has Devastated the World; Should We Prepare for the Outbreak of a New Pandemic? Ann Med Surg. 2022;79:104051.
Crossref - Baack S, Alfred D. Nurses’ Preparedness and Perceived Competence in Managing Disasters. J Nurs Scholarsh. 2013;45(3):281-287.
Crossref - Morse SS. Public Health Surveillance and Infectious Disease Detection. Biosecur Bioterror. 2012;10(1):6-16.
Crossref - Jezek Z, Grab B, Paluku KM, Szczeniowski MV. Human Monkeypox: Disease Pattern, Incidence and Attack Rates in a Rural Area of Northern Zaire. Trop Geogr Med. 1988;40(2):73-83.
- Reynolds MG, McCollum AM, Nguete B, Lushima RS, Petersen BW. Improving the Care and Treatment of Monkeypox Patients in Low-Resource Settings: Applying Evidence from Contemporary Biomedical and Smallpox Biodefense Research. Viruses. 2017;9(12):380.
Crossref - WHO. Monkeypox. https://www.who.int/news-room/fact-sheets/detail/monkeypox. Accessed 2022-09-17.
- CDC. Monkeypox in the U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-healthcare.html. Accessed 2022-09-29.
- Monkeypox. https://www.hopkinsmedicine.org/health/conditions-and-diseases/monkeypox. Accessed 2022-09-17.
- Zoonotic Diseases. One Health. CDC. https://www.cdc.gov/onehealth/basics/zoonotic-diseases.html. Accessed 2022-09-29.
- Damian AJ, Gonzalez M, Oo M, Anderson D. A National Study of Community Health Centers’ Readiness to Address COVID-19. J Am Board Fam Med. 2021;34(Supplement):S85-S94.
Crossref - Adams JG, Walls RM. Supporting the Health Care Workforce During the COVID-19 Global Epidemic. JAMA. 2020;323(15):1439-1440.
Crossref - Huy NV, Bang K-S, Xuan HTA, et al. The Roles of, Activities of, and Competencies for, Community Nursing Services in Rural Vietnam: Implications for Policy Decisions. Int J Health Plann Manage. 2018;33(4):e1147-e1159.
Crossref - Pisano Gonzalez MM, Gonzalez Pisano AC, Abad Bassols A. Community and Family Nurse: Present Keys, Future Challenges. Enfermeria Clinica (English Edition). 2019;29(6):364-368.
Crossref - Clari M, Luciani M, Conti A, et al. The Impact of the COVID-19 Pandemic on Nursing Care: A Cross-Sectional Survey-Based Study. J Pers Med. 2021;11(10):945.
Crossref - Quigley DD, Dick A, Agarwal M, Jones KM, Mody L, Stone PW. COVID-19 Preparedness in Nursing Homes in the Midst of the Pandemic. J Am Geriatr Soc. 2020;68(6):1164-1166.
Crossref - Liu Q, Luo D, Haase JE, et al. The Experiences of Health-Care Providers during the COVID-19 Crisis in China: A Qualitative Study. Lancet Glob Health. 2020;8(6):e790-e798.
Crossref - Akbar MA, Juniarti N, Yamin A. The Roles of Community Health Nurses’ in Covid-19 Management in Indonesia: A Qualitative Study. Int J Community Based Nurs Midwifery. 2022;10(2):96-109.
Crossref
© The Author(s) 2022. Open Access. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License which permits unrestricted use, sharing, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.